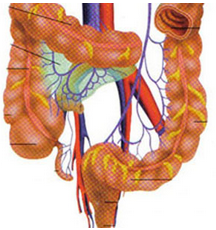
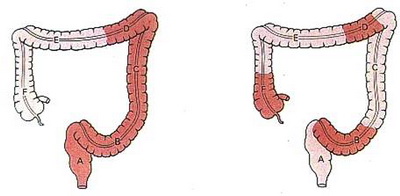
盘点:近期结直肠癌重要研究成果一览
2016-09-19 MedSci MedSci原创
近期结直肠癌研究领域的大量基础和临床研究,从不同方向、不同角度对结直肠癌及其并发症的临床诊治进行了深入研究,为结直肠癌的临床管理寻找最新方向。本文梅斯医学小编就近期结直肠癌领域重要研究成果进行回顾。【1】Lancet Oncol:RAS野生型结直肠癌:FOLFIRI+西妥昔 vs FOLFIRI+贝伐珠(FIRE-3)FIRE-3试验对KRAS外显子2野生型转移性结直肠癌患者的两种治疗方案进行
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究成果#
48
总结的很好!
77
分享一下!
68
#结直肠#
66
有新进展
72
学习啦,,,
86
学习起来
89