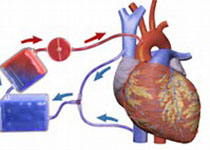
冠心病、脑梗、肾萎缩,从一个病例认识动脉粥样硬化
2017-11-09 李青 李青大夫
一个70岁的老人,半年前开始间断出现心前区疼痛,每次持续大约10分钟,休息后缓解。最近发作比较频繁,于是入住心内科准备行冠脉造影检查。但住院后发现他的血肌酐升高、中度肾衰竭,担心造影剂加重肾衰竭而作罢,随后转入肾内科治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#萎缩#
73
#粥样硬化#
77
#脑梗#
64
是很好的学习材料.不错.以后会多学习.
102
谢谢分享.学习了
112
学习
102
好知识.值得学习
82
学习了提高了
81
很好的文章.谢谢分享
60
看来要系统的看问题
58