JAHA:成人法洛四联症右心房高压的病理生理和预后意义
2019-11-29 xiangting MedSci原创
在症状性TOF患者中,RAP升高与疾病严重程度的多个指标相关(风险分层),并预测未来的心血管事件(预后)
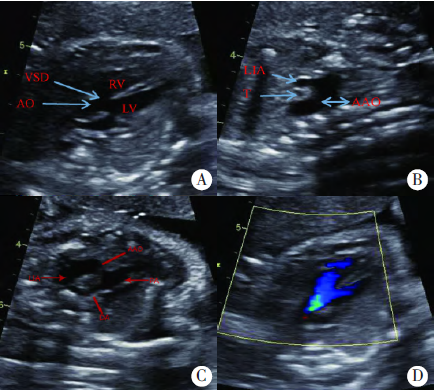
右房压(RAP)是右心室舒张功能、容量状态和右心顺应性的综合指标,可以预测获得性心脏病所致心衰患者的死亡率。法洛四联症患者(TOF)由于心肌损伤和重塑可能存在右心房和心室力学异常,这里假设在该人群中,RAP与疾病严重程度和心血管不良事件有关。
这是一项针对成年TOF患者的队列研究,这些患者在1990年至2017年间于罗切斯特梅奥诊所接受了右心导管检查。目标是确定RAP与TOF多个疾病严重程度方面(占峰值耗氧量预计值百分比、房性或室性心律失常、心衰住院)和心血管不良事件的关联,心血管不良事件定义为持续性室性心动过速、复苏或猝死、心脏移植或死亡。
在225名患者中(113名男性;平均年龄:39±14岁),平均RAP为10.7±5.2mmHg,中位数为10mmHg(四分位范围:7-13mmHg)。RAP每升高5mmHg与房性或室性心律失常(比值比:5.01; 95%CI,1.22–23.49; P<0.001)、心衰住院(比值比:1.47; 95%CI,1.10–2.39; P=0.033)、和运动能力下降相关(峰值耗氧量;R2=0.74,r= 0.86,P<0.001)。RAP每5mmHg是心血管不良事件的预测因子(比值比:1.28; 95%CI,1.10-1.47;P = 0.028)。
在症状性TOF患者中,RAP升高与疾病严重程度的多个指标相关(风险分层),并预测未来的心血管事件(预后)。这些数据对有症状的目标人群具有潜在的临床意义。
原始出处:
Alexander
C. Egbe. Pathophysiologic and Prognostic Implications of Right Atrial
Hypertension in Adults With Tetralogy of Fallot. JAHA. Nov 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#右心房#
78
#病理生理#
63
#AHA#
57
#法洛四联症#
73
#预后意义#
65
#心房#
66