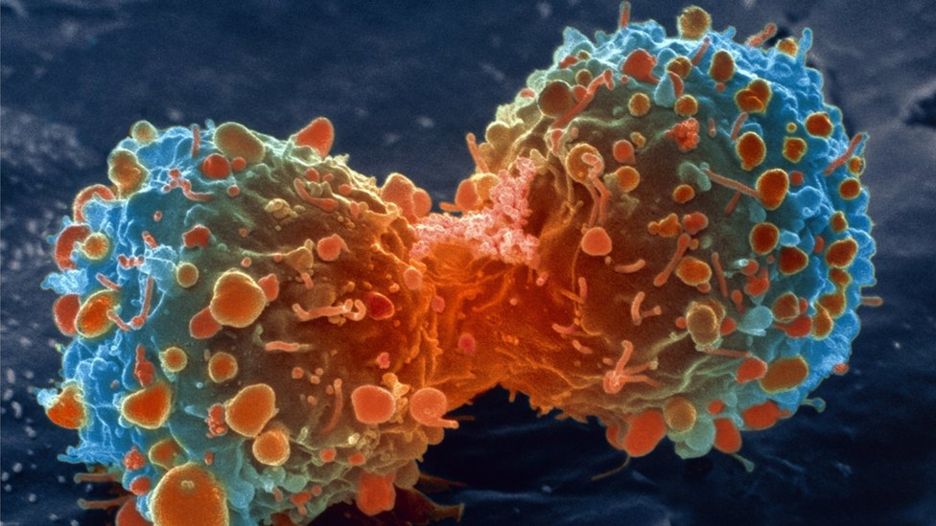
NAT CELL BIOL:为了生存,癌细胞“悄然”改变生物钟
2018-01-02 佚名 生物探索
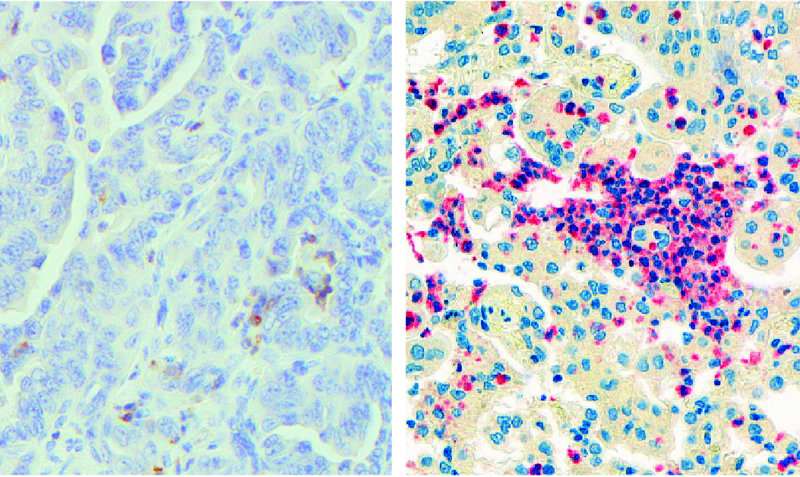
细胞作为构成生物体的基本单位,每一个都拥有自己的生物钟。但是,对于肿瘤细胞而言,其昼夜节律却有所改变。近日,《Nature Cell Biology》期刊在线发表了一篇文章,第一次揭示癌细胞改变昼夜节律、促进扩增的机制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cell#
46
#Bio#
55
#CEL#
39
#Nat#
49
#Biol#
55
学习了新知识
88
#癌细胞#
54
学习了新知识
71