我国研制出全球首台癌症早期检测设备 5分钟检测是否得癌症
2016-04-29 佚名 中国新闻网
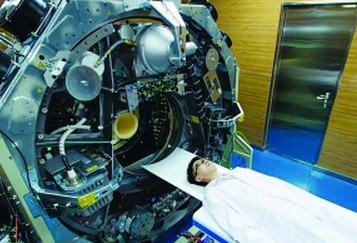
图片来源:武汉晨报 杨佳峰 摄 中国一科研团队27日宣称,研制出全球首台适用于人体全身的临床全数字“正电子发射断层成像仪”(简称“PET”),可精准检测到最小尺寸病灶,大幅提前癌症发现时间。 该成果来源于华中科技大学首个国家重大科学仪器设备开发项目“超高分辨率PET的开发和应用”,由武汉光电国家实验室(筹)研究员、华中科技大学生命学院教授谢庆国带队完成。 PET是继超声
 图片来源:武汉晨报 杨佳峰 摄
图片来源:武汉晨报 杨佳峰 摄
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













深度好文,值得关注
93
这个,标题好厉害的样子,可惜没看到厉害在什么地方,除了自主,,,
96
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
95
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
102
学习了,很好的
133
运用到临床了
105
应该还没有吧
91
些医院有啊?
103
在
159
可靠(* ̄m ̄)
97