JMCB:中国科学家应用CRISPR破解基因组“未解之谜”
2015-08-14 佚名 生物谷
近日,来自上海交通大学的研究人员在国际学术期刊JMCB发表了一项最新研究进展,他们发现应用CRISPR/Cas9技术可以轻松实现对DNA片段的倒位和重复,对于基因组中存在的大量DNA调控元件和大量基因簇的功能研究具有一定意义。研究人员指出,人类基因组中包含了几百万个DNA调控元件和大量的基因簇,但其中大部分都没有进行过实验检测,还有大量基因组"未解之谜"等待人类去破解。DNA编辑技术CRISPR/
近日,来自上海交通大学的研究人员在国际学术期刊JMCB发表了一项最新研究进展,他们发现应用CRISPR/Cas9技术可以轻松实现对DNA片段的倒位和重复,对于基因组中存在的大量DNA调控元件和大量基因簇的功能研究具有一定意义。
研究人员指出,人类基因组中包含了几百万个DNA调控元件和大量的基因簇,但其中大部分都没有进行过实验检测,还有大量基因组"未解之谜"等待人类去破解。
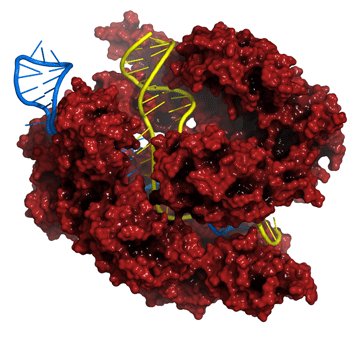
DNA编辑技术CRISPR/CAS9近年来风生水起,该系统是目前发现存在于大多数细菌与所有的古菌中的一种后天免疫系统。由于CRISPR/Cas技术作为一种最新涌现的基因组编辑工具,能够完成RNA导向的DNA识别及编辑,为构建更高效的基因定点修饰技术提供了全新的平台,受到众多科学家的追捧。
在该项研究中,研究人员利用CRISPR系统和两条sgRNA在人类和小鼠的基因组中轻松实现对靶向DNA片段的倒位和重复。研究人员利用该技术可以在培养的人类细胞和小鼠中对几十bp到几千kb大小的DNA片段实现高效精确倒位。同时通过两条同源染色体上Cas9诱导的双链断裂,利用CRISPR技术还可以实现DNA片段的重复和删除。除此之外,研究人员还利用CRISPR技术获得了携带精确倒位,重复和删除不同尺寸DNA片段的等位基因的小鼠。
最后,为证明该技术在DNA调控元件功能研究方面的作用,研究人员将CRISPR方法应用到Pcdhα基因簇的调控元件功能研究中,发现了对Pcdhγ基因簇成员调控的新功能。
总的来说,这项研究表明应用CRISPR/Cas9这种简单高效的方法能够大大促进对DNA调控元件及基因簇功能的研究,这对于破解人类基因组中的大量"未解之谜"具有很大助益。
原文出处:
Jinhuan Li, Jia Shou1, Ya Guo, Yuanxiao Tang.et al.Efficient inversions and duplications of mammalian regulatory DNA elements and gene clusters by CRISPR/Cas9.JMCB.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#中国科学#
59
#JMCB#
59
#CRISPR#
39
#中国科学家#
61
这个研究的报道稍微有些夸张,应该要实事求是,一些会比较合适
72