Nat Commun:重磅级研究!科学家发现HIV病毒的寿命已经5亿岁了
2017-01-12 佚名 生物谷
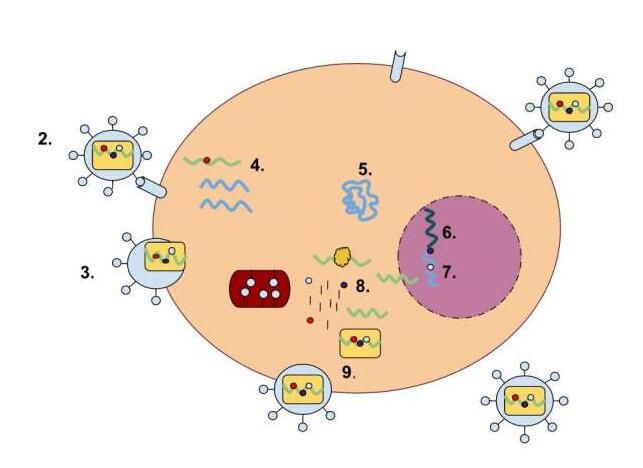
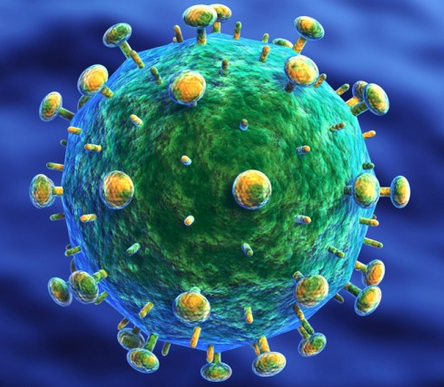
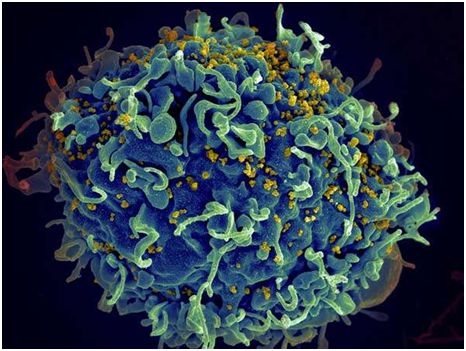
图片来源:www.phys.org 近日,发表在国际杂志Nature Communications上的一项研究报告中,来自牛津大学的研究人员通过研究表示,包括HIV在内的逆转录病毒或许已经有5亿岁了,这要比科学家们此前认为的寿命还要老很多年,而且研究者认为,逆转录病毒或许起源于古代海洋,而且其实随着动物宿主慢慢实现了从海洋到陆地的转变。 本文研究为科学家们理解病毒和其宿主之间的“军

图片来源:www.phys.org
近日,发表在国际杂志Nature Communications上的一项研究报告中,来自牛津大学的研究人员通过研究表示,包括HIV在内的逆转录病毒或许已经有5亿岁了,这要比科学家们此前认为的寿命还要老很多年,而且研究者认为,逆转录病毒或许起源于古代海洋,而且其实随着动物宿主慢慢实现了从海洋到陆地的转变。
本文研究为科学家们理解病毒和其宿主之间的“军备竞赛”提供了新的线索,研究者Aris Katzourakis博士指出,关于逆转录病毒的起源我们并不是很清楚,部分是因为缺少地质华师的记录,逆转录病毒广泛分布于脊椎动物中,同时其还可以在宿主之间互相传播,最终引发新的疾病,比如HIV等,而且逆转录病毒还能够在不同宿主之间实现跳跃性变化,截至目前为止,研究者仍然认为这类病毒是“新手”(只有1亿岁)。
本文研究表明,逆转录病毒至少有4.5亿岁,其是一类包括HIV等病毒在内的一类病毒家族,能够引发多种癌症和免疫缺陷疾病;研究人员利用内源性逆转录病毒的基因组序列进行研究,这些内源性逆转录病毒能够进行组装形成“泡沫”病毒,这类病毒在哺乳动物机体中广泛存在,而且文章中研究人员在多样化的宿主中发现了泡沫样逆转录病毒的基因组化石,比如两栖动物和辐鰭鱼。
研究者Katzourakis指出,本文研究中我们阐明了对医学研究非常重要的病毒至少有5亿岁,这远比我们想象之中要长得多,这对于我们后期理解病毒的起源以及同宿主之间的相互作用提供了一定的线索,当然基于本文研究我们还能够理解脊椎动物如何抵御病毒;随着我们对病毒和宿主免疫机制之间相互作用的深入理解,未来我们也能更加微妙地介入二者之间的平衡来开发出抵御多种疾病的新型疗法和干预措施。
如今当研究者构建出感染人类的多样化病毒的清晰图像时,他们距离揭开病毒的真实面目又近了一步。
原始出处
Pakorn Aiewsakun & Aris Katzourakis.Marine origin of retroviruses in the early Palaeozoic Era.Nat Commun.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
63
#COMMUN#
63
#科学家发现#
55
#HIV病毒#
73
#重磅#
71