我国3D打印人体植入物获批
2015-09-08 刘婧婷 人民网
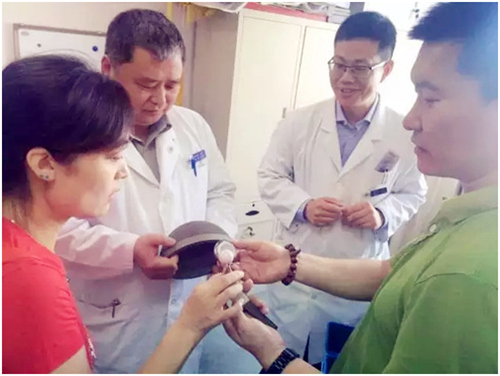
近日,我国首个3D打印人体植入物——人工髋关节产品获得国家食品药品监督管理总局注册批准,该产品也是国际上首个通过临床验证后获得注册的3D打印人工髋关节假体。本次获得注册的人工髋关节产品属于三类骨科植入物是我国监管等级最高的医疗器械产品。该产品由北京大学第三医院骨科医生张克、刘忠军、蔡宏与北京爱康宜诚医疗器材股份有限公司合作研制。曾主刀完成世界首例应用3D打印技术人工定制枢椎治疗寰枢椎恶性肿瘤的北京
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












推广应用
194
#3D#
0
#植入物#
66
#植入#
60