Eur Urol:ATM缺失的晚期前列腺癌:PARP和ATR抑制剂
2020-12-13 AlexYang MedSci原创
之前的研究在转移性前列腺癌(PC)中发现了有害的ATM变异;PARP抑制对该亚型前列腺癌具有抗肿瘤活性,但只有一些ATM缺失的PC有响应。
之前的研究在转移性前列腺癌(PC)中发现了有害的ATM变异;PARP抑制对该亚型前列腺癌具有抗肿瘤活性,但只有一些ATM缺失的PC有响应。
最近,有研究人员表征了ATM缺失致死PC,并研究了该亚型的合成致死治疗策略。研究结果表明,研究人员在68/631(11%)PC患者的至少一次活检中检测到ATM IHC缺失,且存在同步和异时的患者内异质性;46/71(65%)的有ATM缺失的活检通过NGS检测存在ATM突变或缺失。ATM IHC缺失与晚期疾病的更差结果无关,但ATM缺失与基因组不稳定性的增加有关(NtAI:等位基因不平衡延伸至端粒的亚染色体区域数,P=0.005;大规模转换,P=0.05)。在体外,ATM缺失PC模型对ATR抑制敏感,但对PARP抑制的敏感性不一;在这些模型中,PARP和ATR抑制联用可以得到优越的抗肿瘤活性。
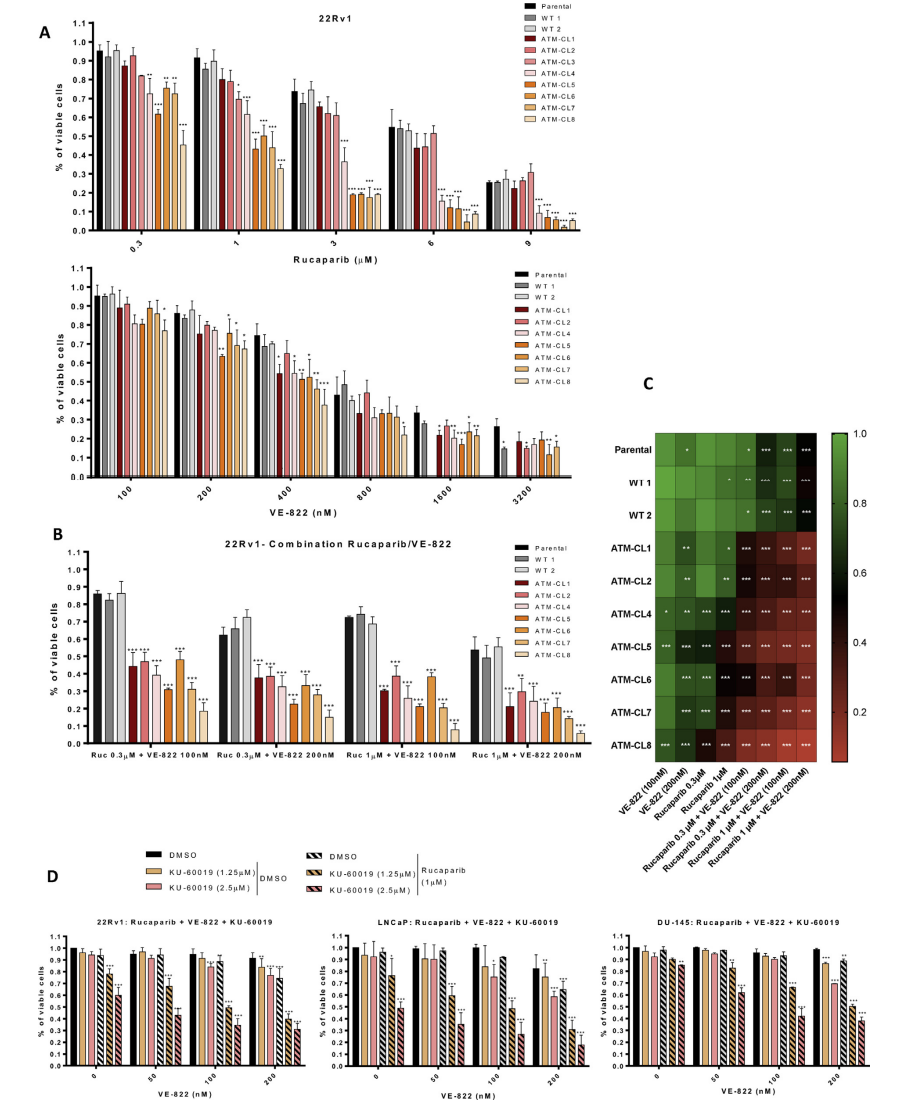
前列腺癌细胞系模型中ATM缺失和对PARP和ATR抑制剂单用或联用的敏感性
最后,研究人员指出,PC中的ATM缺失并不总是能用靶向NGS检测到,且与基因组不稳定有关,并且对ATR和PARP联合抑制最为敏感。
原始出处:
Antje Neeb , Nicolás Herranz , Sara Arce-Gallego et al. Advanced Prostate Cancer with ATM Loss: PARP and ATR Inhibitors. Eur Urol. Nov 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
61
#期前列腺癌#
49
#晚期前列腺癌#
89
#PARP#
78
前列腺癌相关研究,学习了,谢谢梅斯
87
学习了!
112