European Radiology:仅仅看到脑白质高信号还不够,它的分布模式你知道吗?
2022-02-18 shaosai MedSci原创
根据每个病人的WMH分布控制风险因素以达到有助于改善SVD的二级预防。
 在常规MRI中看到的血管来源的白质高信号(WMH)表现常被解释为老年人小血管病变(SVD)的标志,与脑血管危险因素(CVRF)有关,特别是与高血压有关,并与认知能力下降、残疾和卒中风险增加有关。此外,WMH的程度与卒中史、卒中复发、梗塞扩大和急性缺血性卒中(IS)后的不良临床预后有关。
在常规MRI中看到的血管来源的白质高信号(WMH)表现常被解释为老年人小血管病变(SVD)的标志,与脑血管危险因素(CVRF)有关,特别是与高血压有关,并与认知能力下降、残疾和卒中风险增加有关。此外,WMH的程度与卒中史、卒中复发、梗塞扩大和急性缺血性卒中(IS)后的不良临床预后有关。
WMH的严重程度和分布可以通过体积图像分析进行评估。在临床实践中,有几种视觉评分方法,Fazekas量表是使用最广泛的方法之一。大多数目测量表常将脑室上WMH分布分为两大类:脑室周围WMH(PV-WMH),与脑室系统壁相邻;深部WMH(D-WMH),位于远离脑室的皮质下白质。然而在临床上,这些解剖学分布模式的分析及解释尚未达成一致。
近日,发表在European Radiology杂志的一项研究评估了WMH不同区域分布与主要CVRF之间的重要联系,为进一步阐明WMH解剖学模式与不同的病理生理机制之间的关系提供有价值的参考依据。
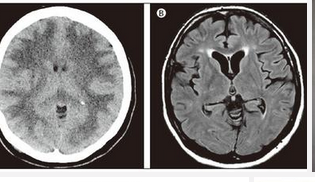
本研究收集了两个独立队列的近期IS患者的临床数据和影像学结果。使用Fazekas、Wahlund和Van Swieten的改良视觉量表评估MRI扫描结果。WMH分布在脑室周围(PV-WMH)和深部(D-WMH)白质、基底神经节(BG-WMH)和脑干(B-WMH)中分别进行分析。还评估了PV-WMH和D-WMH的汇合情况以及WMH的前向和后向优势。统计分析是用SPSS软件进行的。
本研究纳入了618名患者,平均年龄为72岁(标准差[SD]11岁)。最常见的WMH模式是D-WMH(73%)。在多变量分析中,高血压与PV-WMH(几率[OR]1.79,95%置信区间[CI]1.29-2.50,P = 0.001)和BG-WMH(OR 2.13,95% CI 1.19-3.83,P = 0.012)相关。糖尿病与PV-WMH(OR 1.69,95% CI 1.24-2.30,p = 0.001)、D-WMH(OR 1.46,95% CI 1.07-1.49,p = 0.017)以及D-WMH和PV-WMH的综合模式(OR 1.62,95% CI 1.07-2.47,p = 0.024)显著相关。发现高脂血症与脑干分布独立相关(OR 1.70,95% CI 1.08-2.69,p = 0.022)。
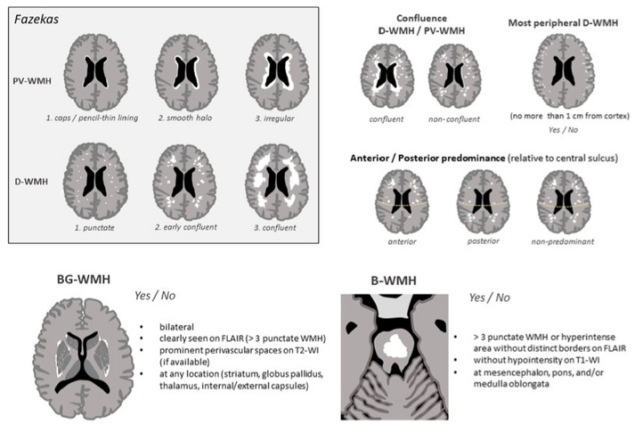
图 神经放射学WMH评价特征。缩略语。WMH=白质增生;D-WMH=深部WMH;PV-WMH=脑室周围WMH;BG-WMH=基底节WMH;B-WMH=脑干WMH;FLAIR=流体衰减反转恢复;T1-WI=T1加权图像;T2-WI=T2加权图像
本研究结果强化了WMH区域分布的不同表型之间关系的存在,并表明其与不同的病理生理机制关系的存在。本研究结果可以转化为常规检查的一部分,根据每个病人的WMH分布控制风险因素以达到有助于改善SVD的二级预防。
原文出处:
Santiago Medrano-Martorell,Jaume Capellades,Jordi Jiménez-Conde,et al.Risk factors analysis according to regional distribution of white matter hyperintensities in a stroke cohort.DOI:10.1007/s00330-021-08106-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#分布模式#
77
#高信号#
74
#PE#
69
#白质#
70
#白质高信号#
66
#脑白质高信号#
118