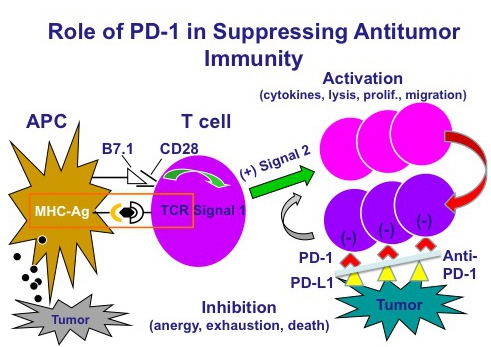
PD-1抑制剂对晚期鳞状非小细胞肺癌具有极其显著疗效,优于紫杉醇化疗
2015-01-13 MedSci MedSci原创
Bristol-Myers Squibb最新PD1抑制药物ornivolumab(Opdivo),原本用于黑色素瘤,最新一项研究用于鳞状非小细胞肺癌的结果显示,在总生存期方面显著优于传统的化疗药物紫杉醇,该试验在早期阶段即中止研究,所有对照组患者全部转向ornivolumab治疗。这项研究给鳞状非小细胞肺癌的治疗带来巨大的变化,这是鳞状非小细胞肺癌近几十年来最大的突破之一。该药物有望被FDA优先审
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抑制剂#
53
#非小细胞#
43
EN
124
#PD-1抑制剂#
48
breaking news
149
PD-1和PD-L1抑制剂将开创肿瘤治疗的新纪元,对以往很多疗效不佳的肿瘤,可能都能展示出独特的疗效
172