视频来自Nature网站
许多遗传和环境因素都可导致肿瘤发生。举个例子,来自太阳的紫外线可能会损伤黑色素细胞(皮肤中的色素生成细胞)中的DNA及其他结构。紫外线对黑色素细胞的慢性损伤是皮肤癌常见类型之一——黑色素瘤的主要诱因。黑色素瘤如果进一步生长,便有可能扩散至身体的其他部位,比如肝和肺。

人体的免疫细胞会对各种组织保持持续性的监视。自然杀伤细胞可以监测到由受损癌变细胞产生的胁迫相关蛋白。树突状细胞可激活细胞毒T细胞,后者可通过其T细胞受体及其他辅助性受体识别肿瘤相关抗原。一旦被激活,自然杀伤细胞和细胞毒T细胞将会释放穿孔素和颗粒酶,这两者可在肿瘤细胞表面制造穿孔,使之凋亡。辅助性T细胞可促进这一过程的发生,通过支持树突状细胞对细胞毒T细胞的激活作用以及产生干扰素-γ等细胞因子,招募和激活更多的自然杀伤细胞。
随着肿瘤的演进,基因突变会不断发生和积累,使得某些肿瘤细胞具备额外的生存优势,并赋予了肿瘤异质性的特点。举例来说,这些基因突变可能使得某些肿瘤细胞不再表达可被免疫杀伤细胞识别的分子。这样,由于逃避了免疫系统的识别,这些肿瘤细胞便快速扩增,且在所有肿瘤细胞中所占比例也逐渐增加。
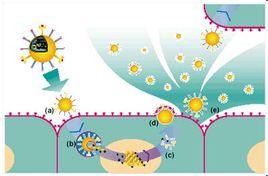
还有一些肿瘤细胞能通过表达PD-L1等分子主动抑制T细胞的功能。PD-L1可结合T细胞表面的PD-1受体从而使后者失活。PD-1在这里这就是免疫检验点。此外,肿瘤细胞还可吸引来一些免疫抑制细胞(包括调节性T细胞和某些髓样细胞)在其周围,从而支持其自身生长。
因此,肿瘤周边的微环境就好像是两种免疫“势力”的战场:一方要攻击肿瘤;另外则一方支持肿瘤生长。科学家们正在开发的癌症免疫疗法就是要加强攻击肿瘤一方的实力。这其中的一种方法就是将黑色素瘤患者体内的细胞毒T细胞分离出来,从中筛选出并扩增对黑色素瘤攻击力最强的细胞群体,再将这些T细胞输送回患者体内,以达到治疗目的。还有一种方法便是引入干扰素-α、白细胞介素-2等细胞因子,以加强抗肿瘤免疫细胞的活性。
当然,我们也可以从免疫检验点入手。例如,抗PD-1抗体可阻止该受体对细胞毒T细胞活性的阻断作用。此外,CTLA-4受体也是一个可作为药物靶点的免疫检验点。如将该受体阻断,则可帮助树突状细胞加强抗肿瘤T细胞的活性。
当然,这类疗法并不是对所有的患者都有效,但若将癌症免疫疗法与放疗、化疗等传统疗法组合在一起,则往往能在一些患者身上取得更好的疗效。不同的癌症免疫疗法之间也可以形成组合治疗方案,比如可将PD-1和CTLA-4同时阻断。
不过,这种将部分免疫功能激活的疗法也是有风险的,可能会在某些患者身上引起有害的副作用,比如导致免疫系统去攻击健康组织。不过,近来的一系列临床试验的结果还是跟人带来希望的。你现在看到的这个视频只是有关黑色素瘤的,而免疫癌症疗法现已被证明可用于治疗多种不同类型的肿瘤。
参考文献
1. Future of Medicine: How Doctors Boost the Immune System to Fight Cancer [Video]
相关会议推荐

2016(第三届)肿瘤与免疫治疗研讨会
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
55
高大上啊
121
值得学习
152
#肿瘤免疫疗法#
71
动画很形象!
123