BMJ:呼吸短促+腹痛+胸部闻及肠鸣音,诊断什么?
2015-11-07 seven L 译 MedSci原创
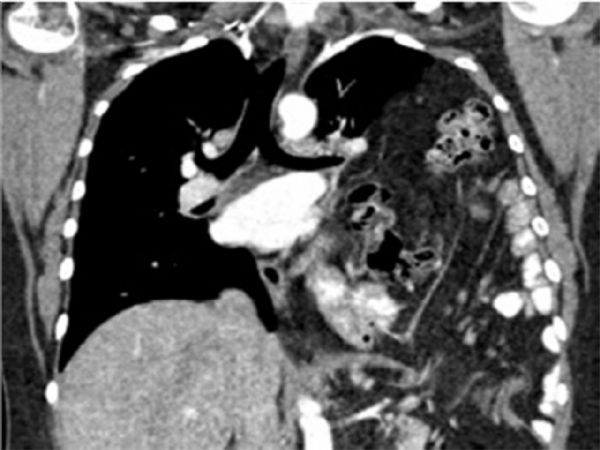
42岁女性,长期呼吸短促且左上腹疼痛。胸部听诊:闻及肠鸣音,且向腋窝传导。胸片:胸腔可见肠段。CT:包含小肠和大肠的膈疝导致肺几乎全部萎缩。膈疝并不是导致呼吸短促的常见原因,不过若呼吸短促患者伴有不具特异性的腹痛症状,则需考虑膈疝。根据临床表现和查体可对该疾病做出初步诊断。该案例也强调了查体的重要性,不鼓励过度依赖影像学检查。原始出处:ames Michael Forsyth,Shariq Sab
42岁女性,长期呼吸短促且左上腹疼痛。
胸部听诊:闻及肠鸣音,且向腋窝传导。
胸片:胸腔可见肠段。
CT:包含小肠和大肠的膈疝导致肺几乎全部萎缩。
膈疝并不是导致呼吸短促的常见原因,不过若呼吸短促患者伴有不具特异性的腹痛症状,则需考虑膈疝。根据临床表现和查体可对该疾病做出初步诊断。该案例也强调了查体的重要性,不鼓励过度依赖影像学检查。
原始出处:
ames Michael Forsyth,Shariq Sabri,et al.Massive diaphragmatic hernia causing shortness of breath and abdominal pain.BMJ 2015;351:h5429
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很好的病例,谢谢分享!
87
有意思,好
73
#BMJ#
40
典型
106
有意思
104
#腹痛#
47