Cancer Cell:肺癌成纤维细胞左右患者对治疗的响应
2021-10-19 haibei MedSci原创
最近,研究人员建立了一个CAFs活体生物库,它来自于非小肺癌(NSCLC)患者的活体组织,包括了临床NSCLC中CAFs的广泛分子谱。
目前的个性化癌症治疗范式主要是基于癌细胞的分子特征,如致癌突变。然而,患者很少实现完全缓解,而且患者反应的深度和持续时间都有很大的差异。目前,人们对于这些差异背后的原因并不完全清楚。癌症相关成纤维细胞(CAFs)之间的功能差异是否在观察到的不同临床反应中起主要作用,以及分析CAF的异质性是否可以改善癌症治疗,都有待确定。
CAFs构成了肿瘤微环境的很大一部分,被认为是癌症生态系统的重要组成部分。最近对包括非小细胞肺癌(NSCLC)在内的实体瘤的单细胞RNA测序(scRNA-seq)研究表明,CAFs是一个具有不同分子特征的细胞集合。此外,在乳腺癌和胰腺癌中已经报道了一些罕见但生物学上独特的成纤维细胞亚型。CAFs的这种多样性引起了人们对利用CAFs改善个性化癌症治疗的日益关注。然而,CAFs的功能在多大程度上是不同的,不同的CAFs可能有什么样的临床影响,在很大程度上仍然是未知的。

缺乏对CAFs功能异质性的全面了解阻碍了更多个性化癌症治疗的发展,以前基于各种CAF定义的研究也产生了不一致的结果。同样,以前试图普遍地针对和广泛地消耗CAF,很少能改善病人的结果。因此,人们目前仍不清楚是否以及如何根据CAF的异质性来制定改进的治疗策略。要回答这些问题,关键是要充分了解特定癌症类型中广泛的CAFs的功能基础,以及它们对该癌症类型当前治疗的影响。
肺癌成纤维细胞的三种亚型确定了不同的治疗范式
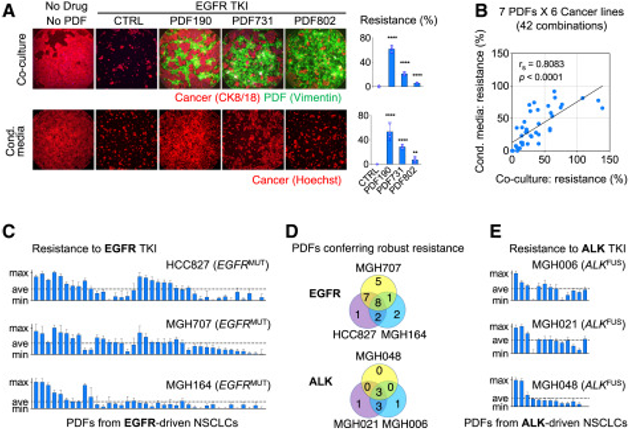
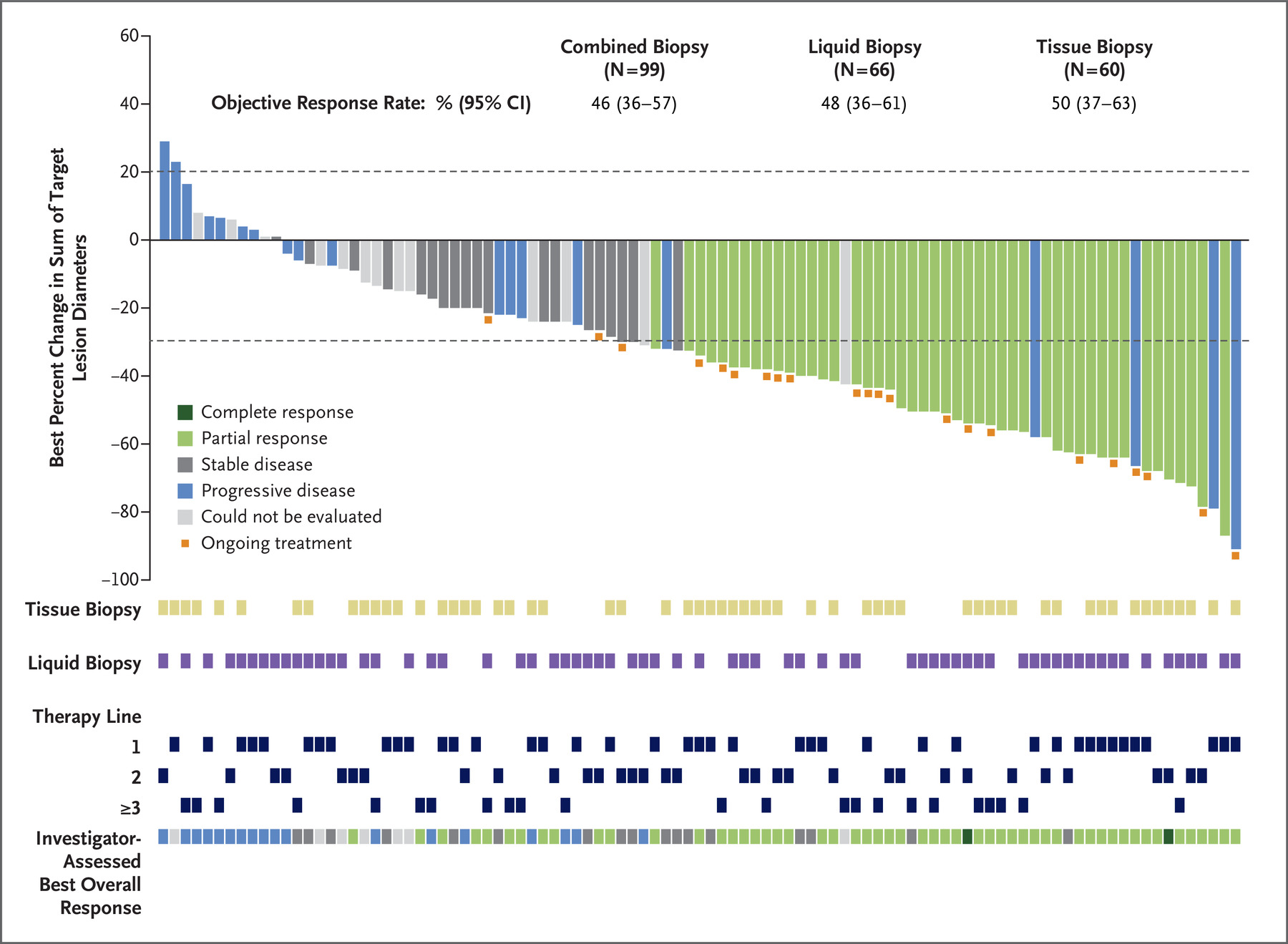
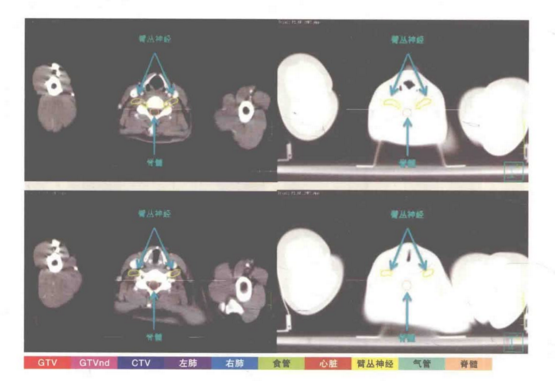
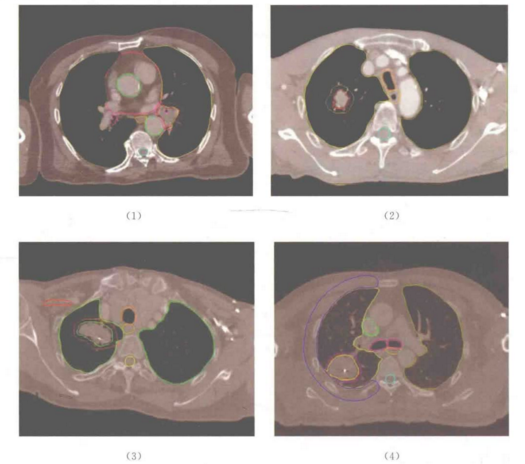
最近,研究人员建立了一个CAFs活体生物库,它来自于非小肺癌(NSCLC)患者的活体组织,包括了临床NSCLC中CAFs的广泛分子谱。通过使用患者接受的相同治疗方法对CAF的异质性进行功能检测,研究人员确定了三种功能亚型,分别为(1)对癌症有强有力的保护作用,并高度表达HGF和FGF7;(2)对癌症有中等程度的保护作用,并高度表达FGF7;(3)对癌症提供最低限度的保护。CAFs之间的这些功能差异受其固有的TGF-β信号的支配,TGF-β信号抑制HGF和FGF7的表达。
此外,这种CAF功能分类与患者对靶向治疗的临床反应相关,也与肿瘤免疫微环境相关,因此提供了一个指导个性化治疗的途径。
原始出处:
Haichuan Hu et al. Three subtypes of lung cancer fibroblasts define distinct therapeutic paradigms. Cancer Cell (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
82
#cancer cell#
104
#CEL#
80
#成纤维细胞#
86
#纤维细胞#
86