The Oncologist: FTD/TPI和瑞戈非尼治疗晚期结直肠癌患者疗效对比
2021-10-03 yd2015 MedSci原创
研究表明,FTD/TPI比瑞戈非尼治疗晚期结直肠癌患者有更好的肿瘤应答率和疾病控制率。
曲氟尿苷盐酸/替吡嘧啶复方片(Trifluridine/Tipiracil ;FTD/TPI或TAS-102)和瑞戈非尼都被批准用于复发/转移结直肠癌的三线治疗。III期临床研究 CORRECT证实,瑞戈非尼较安慰剂改善患者的OS (中位 OS, 6.4 vs. 5.0个月; HR, 0.77; p value =0 .005)。而III期临床研究RECOURSE则证实,FTD/TPI较安慰剂改善患者的OS (中位OS, 7.1 vs. 5.3个月; HR, 0.68; p value <.001)。然而,真实世界中关于两者的疗效以及对比仍然缺乏。因此,美国学者开展了回顾性研究,评估真实世界中晚期结直肠癌患者使用FTD/TPI和瑞戈非尼的疗效对比。相关结果发表在The Oncologist杂志上。
研究纳入2012至 2017年期间符合条件的患者,比较真实世界客观缓解率(rwORR),真实世界疾病控制率(rwDCR),以及生存。
2012年4月至2017年12月,126例患者接受FTD/TPI治疗,95例患者接受瑞戈非尼治疗。接受FTD/TPI治疗的患者中,ECOG 评分为1的患者比例较高(46.8% vs. 32.6%;P= 0.033)。使用瑞戈非尼治疗的患者中,左侧原发性结肠肿瘤的比例较高(57.4% vs. 44.0%;P=0 .049)。首次使用FTD/TPI和瑞戈非尼治疗的患者中位随访时间分别为7.1个月和6.3个月。两组患者在治疗前进行手术的比例相似(FTD/TPI: 65.1% vs. 瑞戈非尼: 75.8%;p=0.086)和手术切除原发肿瘤(FTD/TPI: 61.9% vs. 瑞戈非尼: 73.7%;P= 0.065)。
FTD/TPI治疗较瑞戈非尼治疗的rwORR高(rwORR 52.5% vs. 34.2%; p value =0.012);;同样,FTD/TPI治疗比瑞戈非尼治疗的rwDCR高(rwDCR 64.2% vs. 46.1%; p value = 0.013)。作为二线或三线治疗的患者中,FTD/TPI组比瑞戈非尼组应答更高 (rwORR 54.8% vs. 25.9%;p=0.018),疾病控制率更高(rwDCR 69.0% vs. 37.0%;P=0 .009)。在所有患者中,大多数患者因疾病进展而停止接受FTD/TPI和瑞戈非尼治疗(FTD/TPI: 85.2% vs.瑞戈非尼:77.9%;P=0 .162)。由于毒性/不耐受,FTD/TPI组因毒性或不能耐受停用的比例较瑞戈非尼治疗少(8.2% vs. 24.2%;p<0.001)。
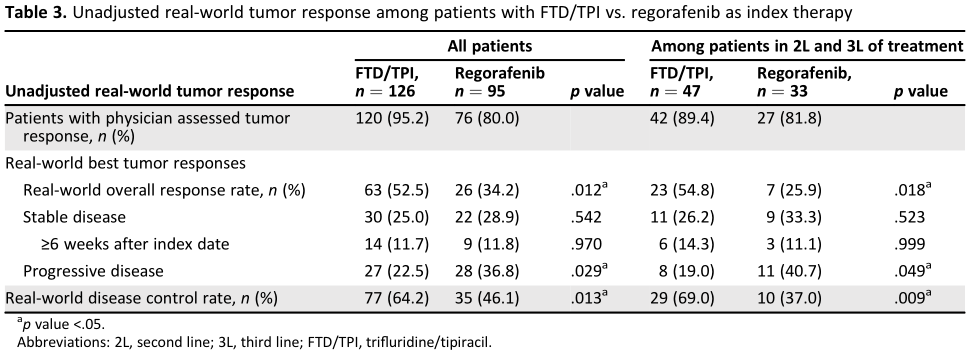
疗效评估
所有接受FTD/TPI治疗和瑞戈非尼治疗患者的中位OS分别为7.5个月(95% CI, 6.0-8.8)和7.1个月(95% CI, 5.0-8.2)。亚组分析,作为二线或三线治疗时,两组的中位OS分别为7.7个月(95% CI, 4.4-11.5)和5.1个月(95% CI, 2.9-7.9),无统计学差异。与瑞戈非尼相比,FTD/TPI治疗的患者3个月 (86.2% vs. 73.4%;P=0 .016)和4个月(79.6% vs. 65.8%;P=0 .017) 存活率更高。经调整后FTD/TPI与瑞戈非尼治疗OS的HR比值为0.80,仍然没有统计学差异(p= 0.157)。

OS
与瑞戈非尼治疗相比,FTD/TPI治疗患者的血液学毒性发生率更高,尤其是中性粒细胞减少的发生率(IRR=5.35;95%CI, 2.01-14.21)。
综上,研究表明,FTD/TPI比瑞戈非尼治疗晚期结直肠癌患者有更好的肿瘤应答率和疾病控制率。
原始出处:
Patel AK, Abhyankar R, Brais LK, Duh MS, Barghout VE, Huynh L, Yenikomshian MA, Ng K, Fuchs CS. Trifluridine/Tipiracil and Regorafenib in Patients with Metastatic Colorectal Cancer: A Retrospective Study at a Tertiary Oncology Center. Oncologist. 2021 Aug 18. doi: 10.1002/onco.13942. Epub ahead of print. PMID: 34406678.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#晚期结直肠癌#
75
#Oncol#
67
#FTD/TPI#
68
好
88
#结直肠#
65
#GIST#
66
#FTD#
71
学习了,谢谢分享
85
直肠癌的一种治疗方法,我学习到了。
72