FASEB J:天津神经病学研究所新发现:改善脑溢血的已批准药物
2017-04-20 李华芸 生物通
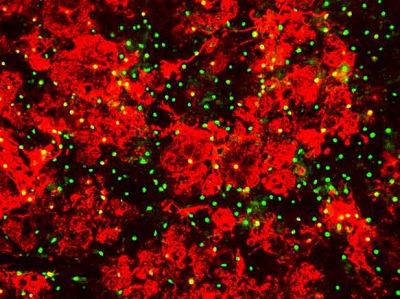
脑溢血(intracerebral hemorrhage ,ICH)是一种严重的中风疾病,脑部血管爆发性的出血,引发威胁生命的病理性脑水肿和神经炎症。最近,天津医科大学总医院、神经病学研究所神经免疫实验室PI刘强博士与耶鲁大学的Fu-Dong Shi博士合作,在美国实验生物学会官方杂志《FASEB Journal》报道了一项具有脑溢血治疗潜力的科学发现。实验发现,一种已知药物艾替伏辛(etifox
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













这类药物对于脑溢血改善如何?我朋友的亲人突发脑溢血
78
#FAS#
67
#新发现#
62
#研究所#
49
#神经病#
105
学习了,不错
138