Neurosurgery: 可应用近红外线成像定位钆增强的胶质瘤
2017-04-20 phylis MedSci原创
背景:由于图像引导系统的应用,术中胶质瘤的实时定位得到很大的改善,但由于脑部移动,手术腔变形及费用等问题,使得这些工具的应用非常有限。目的:基于临床前期及临床研究,研究者在胶质瘤切除术中提出近红外成像方法(NIR),对肿瘤进行定位并识别残留病灶。方法:经食品和药物管理局批准,确定15例患者,在手术前给予NIR造影剂(ICG,5mg/Kg)。在手术前,应用NIR摄像头定位肿瘤并且寻找手术切除边缘。应
背景:由于图像引导系统的应用,术中胶质瘤的实时定位得到很大的改善,但由于脑部移动,手术腔变形及费用等问题,使得这些工具的应用非常有限。
目的:基于临床前期及临床研究,研究者在胶质瘤切除术中提出近红外成像方法(NIR),对肿瘤进行定位并识别残留病灶。
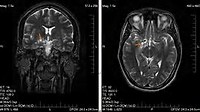
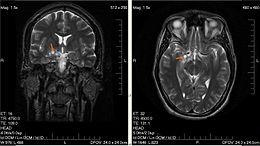
方法:经食品和药物管理局批准,确定15例患者,在手术前给予NIR造影剂(ICG,5mg/Kg)。在手术前,应用NIR摄像头定位肿瘤并且寻找手术切除边缘。应用神经病理学和磁共振成像数据评估应用NIR识别肿瘤组织的准确度和精密度。
结果:静脉注射ICG后, 15例脑胶质瘤患者(10例多形性胶质母细胞瘤、1例间变性星形细胞瘤,2例低级星形细胞瘤,1例少年毛细胞型星形细胞瘤和1例神经节细胞瘤)的NIR可视化平均时间为22.7小时。在手术中, 共有12 例患者应用NIR。信号/背景的平均值为9.5±0.8,且硬脑膜到脑实质的最大深度为13毫米。T1加权增强成像是正荧光最好的预测因子,且与信号/背景比值相关(P =0. 03)。非增强的肿瘤不呈现NIR荧光。如果将病理结果视为金标准,在钆增强组(n = 71),该技术识别肿瘤敏感性为98%,特异性为45%。
结论:随着ICG的使用,可以通过局部脑实质定位钆增强肿瘤。因为其特异性较低,对于肿瘤边缘确定可能会受到限制。
原文出处:
Lee, John Y.K, Thawani, Jayesh P, et al. Intraoperative Near-Infrared Optical Imaging Can Localize Gadolinium-Enhancing Gliomas During Surgery.Neurosurgery,December 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#GER#
71
#近红外#
67
#surgery#
76
#红外线#
68
#ROS#
75