未来5年畅销的抗肿瘤药物TOP10
2016-08-17 风云 健康界
随着肿瘤患者逐年增加,抗肿瘤药物市场也成为近年来医药界关注热点。最新统计显示,全球最畅销的100个药物中抗肿瘤药物有20个。下面来盘点一下未来5年最畅销抗肿瘤药物TOP10,其中既有风骚多年的罗氏三巨头单抗,有持续坚挺的来那度胺,有新型靶向小分子抗癌药物,更有近年来异军突起的PD1抑制剂类药物。TOP1 Revlimid 来那度胺来那度胺是新基(Celgene)开发的新一代抗肿瘤药,主
随着肿瘤患者逐年增加,抗肿瘤药物市场也成为近年来医药界关注热点。最新统计显示,全球最畅销的100个药物中抗肿瘤药物有20个。下面来盘点一下未来5年最畅销抗肿瘤药物TOP10,其中既有风骚多年的罗氏三巨头单抗,有持续坚挺的来那度胺,有新型靶向小分子抗癌药物,更有近年来异军突起的PD1抑制剂类药物。


TOP1 Revlimid 来那度胺
来那度胺是新基(Celgene)开发的新一代抗肿瘤药,主要用于治疗骨髓增生异常综合症和多发性骨髓瘤。它的治疗效果那度胺已获得全球范围内医生和患者的广泛认可。
今年7月份欧盟委员会批准Revlimid用于治疗复发或者难治的套细胞淋巴瘤,FDA批准用于治疗复发或者至少接受过两次治疗的套细胞淋巴瘤;7月份Revlimid用于一线治疗弥散性大B细胞淋巴瘤的III期临床研究也已经结束,其适应症范围将进一步扩大。
来那度胺上市后增长迅速,2015年销售额达58亿美元,而2016年上半年达32.74亿美元,预计2016年销售额将到68亿美元,到2020年它有望成为首个销售额超过百亿美元的抗肿瘤药物,是当之无愧的未来5年最畅销抗肿瘤药物TOP1。
值得一提的是,国内双鹭制药的来那度胺于2016年4月被CFDA纳入优先审批程序,一旦获得批准就表示双鹭的来那度胺成功打破新基来那度胺专利壁垒。
TOP2 Avastin 阿瓦斯汀
阿瓦斯汀作为一种抗血管生成的药物,通过抑制血管内皮生长因子的作用阻断肿瘤,抑制肿瘤在体内扩散,增强化疗疗效。在批准用于治疗乳腺癌前,这种药物还被美国药管局批准用于治疗肺癌、结肠癌和直肠癌,并在欧洲获准用于治疗乳腺癌、结肠癌和直肠癌。相对于赫赛汀和美罗华,阿瓦斯卡面对的生物仿制药竞争不是很大,前二者在欧洲的专利都已到期,而阿瓦斯汀可以被保护到2022年。2016上半年年销售额为35.74亿美元,同比增长了4%,预计未来几年还有一定的上涨空间。
TOP3 Rituxan 美罗华
美罗华是一种抗CD20单克隆抗体,适应症广泛,用于治疗各种血液肿瘤,还可用于二线治疗类风湿性关节炎,它已连续多年蝉联抗肿瘤药物销售冠军的宝座,不过今年应该就是它的销售巅峰了。此药专利在美国将于2016年9月22日到期,一大波仿制药一旦袭来,美罗华的销量势必会大大下跌。罗氏为此推出了一款新药Gazyva来应对生物仿制药的挑战,今年6月罗氏发布了Gazyva针对滤泡性淋巴瘤最新头对头临床试验结果,显示与美罗华相比,Gazyva能够显着延长既往未接受过治疗的滤泡性淋巴瘤患者的无进展生存期,达到了III期临床试验Gallium的主要终点。2016年上半年销售额为38.28亿美元,同比上升了5%。
TOP4 Herceptin 赫赛汀
赫赛汀是治疗HER2阳性弥散性乳腺癌的黄金标准,最近几年的年销售额一直维持在60亿美元以上,但增长空间有限,市场已达到饱和,美国专利将于2019年到期。就此,罗氏推出了取代赫赛汀的药物——Perjeta,用于抵抗生物仿制药的竞争,但临床研究结果表明Perjeta对HER2阳性的乳腺癌治疗效果并不比赫赛汀优秀,其增长潜力并未达到预期效果。赫赛汀2016年上半年销售额为35.51亿美元,同比增长5%。预计2017年后受仿制药竞争影响,将出现销量下滑。
TOP5 Opdivo 纳武单抗
Opdivo 是百时美施贵宝推出的一款新型的PD-1抑制剂类靶向抗肿瘤药物,是被各路人士看好的一款重磅药物。从2014年以来,它被批准上市的适应症已经多达4个,分别是复发难治的经典型霍奇金淋巴瘤;二线治疗不可切除的黑色素瘤;二线治疗非小细胞肺癌;已经晚期或者转移的肾细胞癌。另外还在两个适应症上获得突破性治疗药物资格:头颈部鳞状细胞癌和尿路上皮癌。Opdivo广泛被认为在竞争激烈的PD-1抑制剂类新型抗肿瘤药物中处于领先地位。而它的销售额也证明了这一点,自2014年上市后销售额直线上升,今年上半年销售额为15.44亿美元,几乎是去年同期的10倍,预测到2022年时其峰值年销售额或将超过100亿美元。
TOP6 Ibrance
Ibrance 是辉瑞研发的一种口服性抗CDK抑制剂,可用于治疗各种癌症,它是全球首个CDK4/8抑制剂。2015 年 2 月 3 日,FDA批准Ibrance用于一线治疗 ER+/HER2- 绝经后晚期乳腺癌;2016年4月,FDA批准Ibrance用于二线治疗治疗ER+/HER2- 绝经后晚期乳腺癌,此次获批将显着扩大Ibrance的患者群体。2016年1月Ibrance被英国药品与健康产业管理局(MHRA )授予“重大创新新药”资格,这意味着Ibrance离进入英国药物快速审批通道EAMS更近了一步,进入英国市场也指日可待。业界对Ibrance的商业前景也十分看好。此前,全球医药行业调研机构GlobalData发布报告指出,辉瑞CDK4/6抑制剂Ibrance将主导HR+乳腺癌。2015年Ibrance 销售量达14.43亿美元,2016年上半年为9.42亿美元,预计销售峰值将超过50亿美元。
TOP7 Imbruvica 依鲁替尼
依鲁替尼是一款新型的BTK酶抑制剂,是由强生和艾伯维共同研发,已被FDA批准用于治疗套细胞淋巴瘤、慢性淋巴细胞白血病、非霍奇金淋巴瘤等,6月份被欧盟批准用于治疗慢性淋巴细胞白血病。处于后期临床研究的适应症包括:弥漫性大B细胞淋巴瘤、滤泡性淋巴瘤、胰腺癌。艾伯维和强生对此药及其乐观,称Imbruvica的年销售峰值可望达到115-120亿美元,这虽然有点过于夸张,但依鲁替尼表现确实强劲,2015年销售为14.43亿美元,2016年上半年销售额已达到13.76亿美元。观察家们预期此药销售峰值可达50亿美元。
TOP8 Keytruda
Keytruda是默沙东推出的一款抗PD1单克隆抗体,也是BMS的Opdivo强有力对手,二者在PD1抑制剂市场上的竞争也颇有看点。2015年10月Keytruda首先被批准治疗肺癌,虽然Keytruda比Opdivo提前上市,但Opdivo后来居上,2015年销售额以9.42亿美元的成绩远超Keytruda的5.66亿美元,2016年上半年销售额更是以15.44亿美元比Keytruda的5.63亿美元扩大战果。但最近的一些消息却让人看到Keytruda对Opdivo的反击,首先是Opdivo一线治疗非小细胞肺癌III期研究失败,然后是Keyturda治疗头颈癌获得FDA的批准。这也让Keytruda的销售前景变得明朗起来,预计到2020年时,Keytruda年销售将达40亿美元。
TOP9 ZYTIGA 阿比特龙
阿比特龙是细胞色素P45017A1(CYP17)的抑制剂,用于治疗前列腺癌。它通过抑制剂CYP17来抑制睾丸酮的生成,从而降低睾丸酮对癌细胞生长的促进作用。自2011年上市后,ZYTIGA一直是治疗前列腺癌药物中的霸主 ,直到2014年安斯泰来Xtandi的出现,ZYTIGA才终止了三年快速增长的阶段,其2015年销售额为22.31亿美元,基本与2014年持平,2016年上半年销售额为11.59亿美元。看来由于竞争对手的压力,此药增长空间有限,预计未来几年销售额将维持在20亿美元左右。
TOP10 Alimta 力比泰
Alimta是一种传统的抗癌药物,其结构上含有核心为吡咯嘧啶基团的抗叶酸制剂,通过破坏细胞内叶酸依赖性的正常代谢过程,抑制细胞复制,从而抑制肿瘤的生长。2004年被FDA批准用于治疗恶性胸膜间皮瘤;2008年被批准用于非小细胞肺癌;2009年用于非小细胞肺癌的长期治疗。Alimta的销售量一直不错,近几年一直维持着20亿以上的年销售额,但随着专利2017年到期,销售额将逐年下滑。2015年销售额24.93亿美元,2016年上半年销售11.71亿美元,预计2018年后年销售额将跌至20亿美元以下。
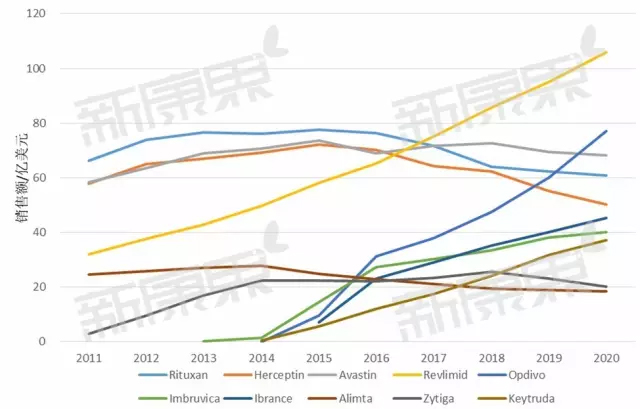
附图:各药物自2011年以来销售情况,2016后是估值
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TOP10#
36
赞了!深度好文,深入学习。
67
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
72
值得学习
69
#肿瘤药物#
50
#肿瘤药#
44
#抗肿瘤药#
45
学习了,赞一个!
68
学习了,赞一个!
75
学习了,赞一个!
37