JBJS:儿童股骨干骨折单腿人字石膏安全有效便于护理
2012-08-07 zhanghaisen 丁香园
对于2-6岁的儿童股骨干骨折,人字石膏固定是其治疗选择之一。但在对这类病例实施人字石膏固定时,采用单腿石膏还是双腿石膏在临床尚未有统一的标准,二者的治疗效果何者更佳也未见相关临床报道。最近,美国约翰·霍普金斯大学医学中心骨科的Leu D等针对这一问题实施了一项前瞻性随机对照研究,其相关研究结果发表于近期出版的JBJS(Am)杂志。该研究的证据级别为治疗性研究I级。 在该研究中,研究者将52例儿童
对于2-6岁的儿童股骨干骨折,人字石膏固定是其治疗选择之一。但在对这类病例实施人字石膏固定时,采用单腿石膏还是双腿石膏在临床尚未有统一的标准,二者的治疗效果何者更佳也未见相关临床报道。最近,美国约翰·霍普金斯大学医学中心骨科的Leu D等针对这一问题实施了一项前瞻性随机对照研究,其相关研究结果发表于近期出版的JBJS(Am)杂志。该研究的证据级别为治疗性研究I级。
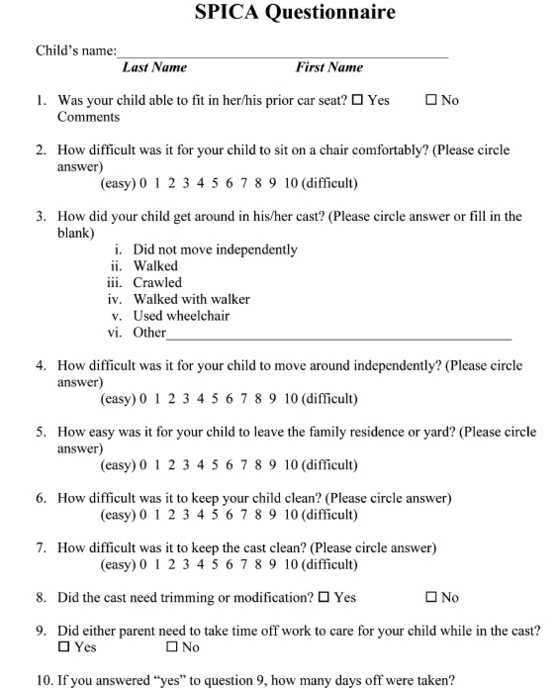
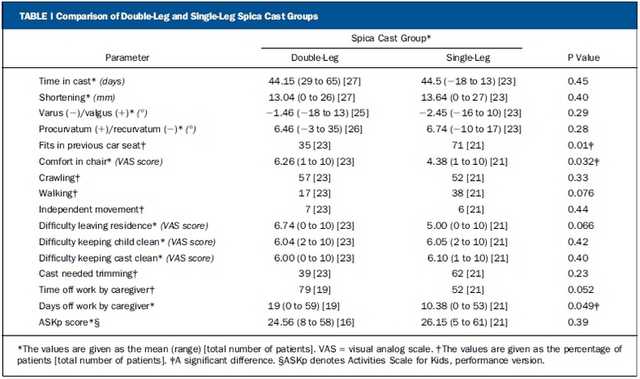
在该研究中,研究者将52例儿童股骨干骨折患者随机分为两个治疗组:单腿人字石膏固定组(24例)和双腿人字石膏固定组(28例)。治疗过程中通过连续拍摄X线片对肢体长度,内/外翻成角,前/后弓成角等骨折复位情况进行评估。石膏固定去除后,采用儿童活动调查评估问卷(Activities Scale for Kids, ASK)及制定的书面调查问卷对患儿治疗期功能和护理工作的易操作性等进行考察。组间比较的统计学方法采用Student t检验。
所以病例骨折均获愈合,复位、对线满意。单腿人字石膏固定的患儿在乘坐汽车以及座椅时更为舒适(p<0.05),其看护者在工作之余花费的时间更少(p<0.05)。两组病例均未出现重大并发症。根据这一研究结果,作者认为,儿童股骨干骨折病例采用单腿人字石膏固定安全、有效,护理更为方便。
原文链接:
Leu D, Sargent MC, Ain MC, Leet AI, Tis JE, Sponseller PD. Spica casting for pediatric femoral fractures: a prospective, randomized controlled study of single-leg versus double-leg spica casts. J Bone Joint Surg Am. 2012 Jul 18;94(14):1259-64.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#股骨干#
67
#骨干骨折#
66
#股骨#
0
#JBJS#
58