NEJM:骨石化症案例报道
2015-09-17 MedSci MedSci原创
一名8岁的男孩因右腿出现急性的疼痛发作而来院就诊。X光片检查显示其右腿股骨干存在稳定性骨折(如图A所示),且可见股骨干远端呈现锥形瓶的畸形(如图B所示)。据了解,该男孩在其出生6个月时曾被诊断患有神经母细胞瘤,但在之后的5年里通过采用环磷酰胺和每个月静脉注射双磷酸盐进行治疗后,症状一直有所缓解。此后停止双磷酸盐治疗18个月,由于担心病情变化进行常规X线成像检查检测,以防演变成骨石化症。实验室检测、
一名8岁的男孩因右腿出现急性的疼痛发作而来院就诊。
X光片检查显示其右腿股骨干存在稳定性骨折(如图A所示),且可见股骨干远端呈现锥形瓶的畸形(如图B所示)。
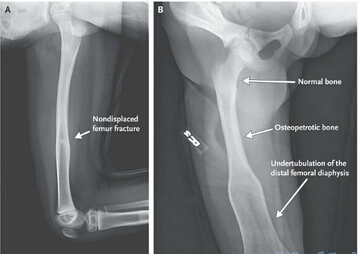
实验室检测、X线成像以及基因检测均无发现任何遗传或其他原因获得性骨疾病,包括原发性骨髓疾病,重金属中毒,骨代谢性疾病,和其他发育不良。
从图B中可见,正常骨段与骨石化段之间的分阶段,呈梯次性生长。而这一现象与骨石化症的表现更加地符合。
目前,病人存在骨石化端与正常骨之间发生骨折的风险,主治医生建议其勿进行强烈的运动,并坚持进行年度随访。
1年半后,该男孩没有出现新的症状和骨折。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









不错,赞一个
128
这篇文章有一定深度
119
是一篇不错的文章
85
值得进一步关注
153
真不错,涨姿势
85
我是骨科医生,很喜欢med的骨科板块,从科普到高端都有
91
真不错,涨姿势
153