Pipeline密网支架治疗颅内复杂动脉瘤显优势
2016-06-04 MedSci MedSci原创
首都医科大学宣武医院神经外科在国内率先开展Pipeline密网支架治疗颅内复杂动脉瘤效果较好,随访结果显示,使用该技术治疗的患者动脉瘤均完全治愈。颅内动脉瘤人群患病率约为7%,复杂颅内动脉瘤包括直径大于25毫米的巨大动脉瘤,以及特殊部位动脉瘤如海绵窦内、床突段,以及颅内动脉扩张等。既往治疗这些疾病的主要手段包括开颅动脉瘤直接夹闭,动脉瘤孤立加搭桥,及介入治疗等,治疗难度高、手术风险大,术后并发症发
首都医科大学宣武医院神经外科在国内率先开展Pipeline密网支架治疗颅内复杂动脉瘤效果较好,随访结果显示,使用该技术治疗的患者动脉瘤均完全治愈。
颅内动脉瘤人群患病率约为7%,复杂颅内动脉瘤包括直径大于25毫米的巨大动脉瘤,以及特殊部位动脉瘤如海绵窦内、床突段,以及颅内动脉扩张等。既往治疗这些疾病的主要手段包括开颅动脉瘤直接夹闭,动脉瘤孤立加搭桥,及介入治疗等,治疗难度高、手术风险大,术后并发症发生率较高。
首都医科大学宣武医院神经外科经过近1年的使用,发现Pipeline密网支架治疗颅内复杂动脉瘤具有操作相对简单,创伤小,无需填塞过多的弹簧圈,术后占位效应小,并发症发生率相对较低等优势。同时,密网支架金属覆盖率较普通支架明显提高,且具有显著的血流导向作用,可减少血流进入动脉瘤腔内。
Pipeline密网支架是一种钴铬镍合金支架系统,为近年来上市的新型血管内栓塞辅助装置。2011年美国 FDA 已批准Pipeline密网支架(PED)用于治疗未破裂的大型和宽颈动脉瘤,但对PED治疗破裂动脉瘤的安全性和有效性尚不明确。美国宾夕法尼亚州托马斯杰斐逊大学杰斐逊神经病学医院神经外科的Nohra Chalouhi等进行了回顾性研究,发现PED治疗破裂动脉瘤安全有效,结果发表于2015年2月的《Neurosurgery》杂志。
该研究的病例纳入标准为 Hunt-Hess分级Ⅰ-Ⅲ级的SAH患者,证实为动脉瘤破裂引起,而且不适合单独采用弹簧圈栓塞或开颅夹闭手术治疗。作者纳入2012年1月至2014年1月期间在托马斯杰斐逊大学医院接受PED治疗的20例破裂动脉瘤患者,其中女性15例,男性5例,年龄介于43~80岁。动脉瘤平均直径为7.2±6.9 mm;其中16例为囊状动脉瘤,4例为夹层动脉瘤。6例动脉瘤位于眼动脉,6例位于颈内动脉床突旁段,5例位于椎基底动脉,1例位于颈内动脉海绵窦段末端,1例位于大脑中动脉,1例位于后交通动脉。Hunt-Hess分级Ⅰ级患者7例,Ⅱ级9例,Ⅲ级4例。
从SAH发生到接受PED治疗的中位时间间隔为2天(0~19天,平均间隔7±7天)。6例患者在PED放置前或PED放置过程中使用了弹簧圈栓塞治疗,4例患者在PED治疗后1-2周内接受弹簧圈辅助栓塞。1例患者在栓塞术中发生动脉瘤再次破裂出血,最终死亡。其它患者术后均未发生脑梗死或再出血,无需行二次治疗。
随访发现全部患者均未出现与PED相关的新发神经功能障碍,预后良好(改良Rankin评分为0-1)。15例患者在治疗后5.3±4.2月(2-12月)接受脑血管造影复查,结果显示12例(80%)动脉瘤完全栓塞,3例(15%)不完全栓塞(图1、图2)。

图1. PED治疗大脑中动脉大型动脉瘤。A. DSA示大脑中动脉大型动脉瘤;B. 首先利用弹簧圈栓塞动脉瘤,但栓塞不完全;C. 住院期间采取后续PED治疗;D. X光片显示PED装置(箭头所示);E. 6个月后DSA显示动脉瘤进一步闭塞,但仍不完全。
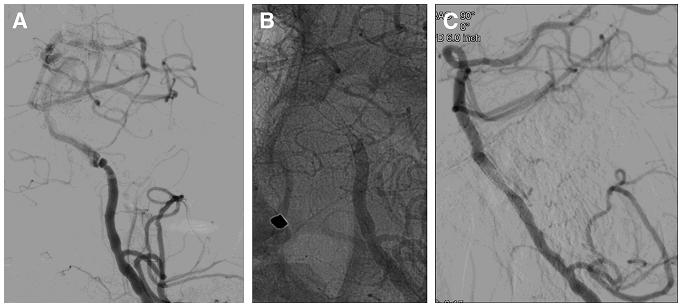
图2. PED治疗椎动脉夹层动脉瘤。A. DSA示左椎动脉V4段夹层动脉瘤;B. PED装置安放于载瘤动脉并通过动脉瘤部;C. 6个月后DSA未见动脉瘤存在。
该研究表明,应用PED治疗破裂动脉瘤并发症少,栓塞效果满意,能显著改善患者预后。因此,PED有望成为可供Hunt-Hess分级较好、传统方法难以完全治愈的动脉瘤患者选择的安全有效的治疗方法。
相关文献:
Daou B, Valle-Giler EP, Chalouhi N, Starke RM, Tjoumakaris S, Hasan D, Rosenwasser RH, Hebert R, Jabbour P.Patency of the posterior communicating artery following treatment with the Pipeline Embolization Device. J Neurosurg. 2016 May 6:1-6.
Daou B, Starke RM, Chalouhi N, Tjoumakaris S, Hasan D, Khoury J, Rosenwasser RH, Jabbour P.Pipeline Embolization Device in the Treatment of Recurrent Previously Stented Cerebral Aneurysms. AJNR Am J Neuroradiol. 2016 May;37(5):849-55.
Daou B, Starke RM, Chalouhi N, Barros G, Tjoumakaris S, Rosenwasser RH, Jabbour P. P2Y12 Reaction Units: Effect on Hemorrhagic and Thromboembolic Complications in Patients With Cerebral Aneurysms Treated With the Pipeline Embolization Device.Neurosurgery. 2016 Jan;78(1):27-33
Chalouhi N, Zanaty M, Whiting A, Tjoumakaris S, Hasan D, Ajiboye N, Hann S, Rosenwasser RH, Jabbour P. Treatment of ruptured intracranial aneurysms with the pipeline embolization device. Neurosurgery. 2015 Feb;76(2):165-72
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#支架治疗#
86
#PE#
77
#PEL#
0
不错的文章,多学习
209
涨知识,学习了
237
厉害!
234
技术而言,国内与国际上还是有差距,这种技术国际上已经使用了不少年头了,国内才刚刚开始
204