JAD:大脑成像新技术MRS有助阿尔茨海默病早期诊断
2012-05-19 科讯网 科讯网
阿尔茨海默症(AD)是主要的神经退行性疾病之一,全球数百万人因该疾病而受到不同程度的影响。寻找新的、更精确的诊断方法对于该疾病的早期诊断尤为关键。 近日,Pravat K. Mandal博士和他的同事们共同研究开发出一种完全无创的大脑成像技术,利用该技术可以测出脑内某些特殊化学物质的变化,这为病变于大脑海马区AD的早期诊断拉开了序曲。研究论文发表于《阿尔茨海默症》杂志(Journal of Al

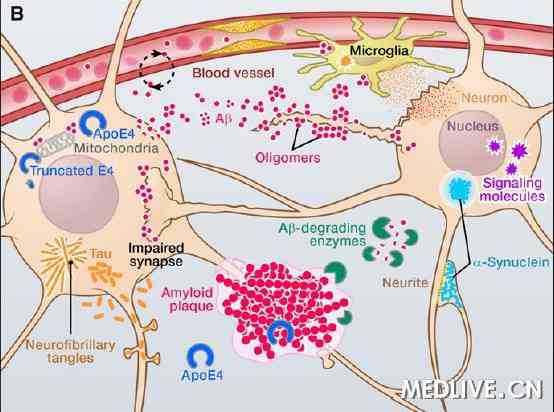
阿尔茨海默症(AD)是主要的神经退行性疾病之一,全球数百万人因该疾病而受到不同程度的影响。寻找新的、更精确的诊断方法对于该疾病的早期诊断尤为关键。
近日,Pravat K. Mandal博士和他的同事们共同研究开发出一种完全无创的大脑成像技术,利用该技术可以测出脑内某些特殊化学物质的变化,这为病变于大脑海马区AD的早期诊断拉开了序曲。研究论文发表于《阿尔茨海默症》杂志(Journal of Alzheimer's Disease)。
联合了印度Gurgaon国家大脑研究中心和约翰霍普金斯大学医学院共同参与此项研究的Mandal说:“在高龄人群中,阿尔茨海默症(AD)已经变成了一场无声的海啸,悄悄席卷而来。这项新开发的诊断技术无需传统的血液检测,也不用接受放射性检查,整个过程只需不超过五分钟即可完成,因此很有可能给诸多的AD患者及其家庭带来新的希望和福音。”
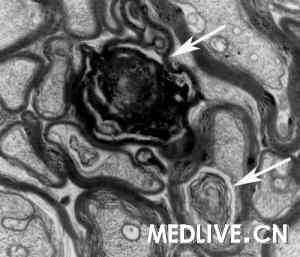
Mandal和他的合作研究者运用三维31P磁共振波谱分析(MRS)成像以及一种先进的分析仪器研究了正常对照组、AD患者组、轻微认知功能障碍(MCI)患者组的大脑,分别对他们的大脑海马区化学物质变化做了评估分析。他们观察到在实施研究的过程中,AD患者的左侧海马变成碱性,而正常年龄增长者当中这一结果却恰恰相反,他们的海马趋向于更酸性。
Mandal博士和他的同事们除此之外还确定了另外四种改变的大脑化学物质,与正常对照组相比,在阿尔茨海默症病变前患者和阿尔茨海默症患者当中,这四种蛋白有显著的改变。这四种蛋白分别为磷酸单酯 (PME)——神经元膜的构成成分;磷酸二酯(PDE)——神经元膜的降解产物;磷酸肌酸(PCr)——为脑功能储备能量;以及三磷酸腺苷(-ATP)——大脑的能量源泉。他们的研究发现在这些病人中的左侧海马区,其PME水平显著下降,而PDE,PCr和-ATP含量水平则增加。
Mandal博士解释说:“伴随着左侧海马区PDE,PCr和-ATP的增加以及PDE含量水平的下降,左侧海马区PH增加至碱性范围内,因此这些物质有可能成为新的AD诊断生物标记物。”他和他的同事们计划下一步对大样本的阿尔茨海默症和帕金森病例实施新的纵向研究,以进一步确定他们目前检测手段的特异性。“这样的临床研究也正是我们所期望的,我们希望能借助这一顶尖水准级的最新检测手段能够较早诊断或更准确地预测AD,这些也许能够给认知功能受损的病人带来新的希望。”

doi:10.3233/JAD-2012-120166
PMC:
PMID:
Mapping of Hippocampal pH and Neurochemicals from in vivo Multi-Voxel 31P Experiments in Healthy Normal Young Male/Female, Mild Cognitive Impairment, and Alzheimer's Disease
Pravat K. Mandal1, Himanshu Akolkar1, Manjari Tripathi2
Magnetic resonance spectroscopy (MRS) plays an important role in the understanding of membrane and energy metabolism. The outcome of MRS experiments helps to derive important cellular conditions (e.g., intracellular pH, energy, membrane metabolism, etc.), which are directly related to neuronal health. We present a novel multi-voxel 31P MRS imaging experimental scheme along with an advanced 31P signal processing technique to determine the pH and neurochemicals from both hippocampal areas in shorter time (13.2 min) for subjects (e.g. healthy young male/female, mild cognitive impairment (MCI) and Alzheimer's disease (AD)). Significant (p = 0.005) decrease of phosphomonoester (PME) and increase of phosphodiester (PDE) (p < 0.001), γ-ATP (0.008), and PCr (p = 0.001) levels in the left hippocampus of AD patients (n = 6) compared to the control subjects (n = 12) were found based on post-hoc ANOVA. On the other hand, in the right hippocampus, decrease in PME (p = 0.008) and increase in PDE (p < 0.001) were significant between AD patients and controls. In case of AD subjects, pH in the left hippocampus is increased towards alkaline side compared to MCI but did not reach statistical significance level. The pH (left hippocampus) in AD is found to be negatively correlated (r = ?0.829, p = 0.042) with PCr level (left hippocampus) in AD subjects. In the left hippocampus, the increase in pH to alkaline range (in normal aging, pH is decreased to acidic range) along with statistically significant increments of PCr, γ-ATP, and PDE as well as decrease of PME in AD subjects provide extremely crucial clinical information, which can be used as biomarker for AD and potentially aid in the diagnosis.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阿尔茨海#
64
#mRS#
69
#大脑成像#
87
#阿尔茨#
51
#脑成像#
66
#新技术#
81
#早期诊断#
58
#阿尔茨海默#
53