路易体痴呆患者,你见到过吗?
2015-11-09 QQduhq 译 MedSci原创
ABC新闻报道,一名名叫苏珊的女性去年一直探索丈夫的死因,近期终于通过验尸官得知,她丈夫死于路易体痴呆(LBD)。且威廉姆斯的解剖专家认为,这是他们见过的最严重的病例。但是为什么不能提早发现呢? 毕竟,路易体痴呆(LBD)是第二大最常见的进行性痴呆,约130万美国人罹患此病,且大多为年龄超过65岁的老人。然而,尽管它如此流行,却也最容易误诊。 根据路易体痴呆协会(LBDA)的调查,平均需要3个
ABC新闻报道,一位名叫苏珊的女性去年一直探索丈夫的死因,近期终于通过验尸官得知,她丈夫死于路易体痴呆(LBD)。且威廉姆斯的解剖专家认为,这是他们见过的最严重的病例。
但是为什么不能提早发现呢?
根据路易体痴呆协会(LBDA)的调查,平均需要3个医生和18个多月的检查才能正确确立LBD的诊断。大多数医生未能认识到老人出现的LBD临床表现,因为LBD老人表现出的症状同老年痴呆症和其他神经退行性疾病如帕金森症等非常相似。
现在,让我们一起来学习路易体痴呆(LBD)这一疾病的成因、疾病的症状和体征、治疗方案,经常误诊的原因,以及如何提高人们对这一潜在威胁的重视。
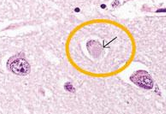
路易体痴呆于20世纪90年代,首次被德国神经学家Freiderich H. Lewy发现。Lewy博士在研究帕金森病时,发现小脑细胞存在一种α-突触核蛋白,后来被命名为路易小体。路易小体存在于帕金森并LBD患者大脑中,但它们位于大脑的不同区域。在帕金森症患者脑中,路易小体主要存在于在黑质区;而LBD患者脑中的路易小体则遍布大脑皮层。虽然目前还不清楚路易小体是如何出现及进展的,但是它们的积聚会导致脑内神经递质水平降低——尤其是乙酰胆碱和多巴胺。
如前所述,LBD的临床表现与帕金森症相似,许多患有帕金森症患者将会出现痴呆相关性记忆和思考问题,而LBD患者则不仅会出现记忆思考问题,也会出现相关运动问题。相似的临床表现使得一些研究人员认为LBD和帕金森症是由大脑对α-突触核蛋白的异常处理所致。
一些LBD和帕金森病患者脑中也会出现β-淀粉样蛋白和tau蛋白等,这是阿尔茨海默病的标志。
路易体痴呆的特殊临床表现:
LBD患者也会出现行为和情绪问题,如焦虑和抑郁等。
大多数人LBD患者出现幻视,少数人会出现幻听表现。约2/3的LBD患者出现类似帕金森症的运动障碍——包括速度减慢、肌肉震颤、拖步走路,且这些表现不断加重。LBD患者出现的另一个表现是睡眠障碍,这主要是由于机体自主神经功能的改变。
但由于没有独自的LBD测试,因此,LBD的诊断只能通过临床评估得知。若许多医生不熟悉LBD的临床表现,这将会导致误诊且延误病情的治疗。
他们通过评估病人的心理能力、抽血液标本、排除维生素缺乏导致的大脑功能减退。通过脑部扫描,如MRI和CT等可以排除脑部肿瘤的存在。但是这些仍然无法明确诊断。目前,只有通过患者死后解剖胆道才可确立LBD诊断。
LBDA最近对近1000名LBD开展调查,他们发现,近80%的患者最初被诊断为不同的神经性疾病,超过50%的患者被误诊为阿尔茨海默氏症。
最近的一项调查显示,患者平均要就诊三个医生才能正确地诊断出患有LBD。更重要的是,15%的患者就诊五名医生才能得出准确诊断。只有27%的LBD患者在出现临床表现的3个月内被正确诊断患有LBD。据调查,23%的患者需要历时1年才可确立诊断。然而,就诊时间超过1年才能得到正确诊断的患者占50%,其中20%的患者甚至需要花费3年时间才可得到准确诊断。
例如,患者出现的运动症状可通常用治疗帕金森症的药物来治疗,而认知症状可用胆碱酯酶抑制剂等药物治疗。也有一些患者通过行为治疗等使症状得以好转。但LBDA强调,对某些药物,LBD患者非常敏感,甚至会导致病情的加重或引起严重的副作用。抗精神病药物治疗会导致患者出现幻觉,也会加重运动障碍。因此,治疗LBD需要全面多学科联合协作,以得到最佳的治疗方案。
虽然目前还没有LBD通用的治疗方案,但研究人员正在努力。Medical News Today最近发表的一项研究表明,对LBD小鼠可通过干细胞移植以改善小鼠的行为及认知障碍。 医务人员也需要提高对LBD的认识程度,并提高意识。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#路易体#
80
#痴呆患者#
53
很不错
210
赞
22
赞
131