Nat Chem Biol:新型抗菌化合物可有效抵御耐药病原体且毒性较低
2015-06-04 佚名 生物谷
靶向攻击真菌感染而不损伤人类细胞的新型化合物或许可以有效避免抗生素耐药性的产生;近日,刊登在国际杂志Nature Chemical Biology上的一篇研究论文中,来自伊利诺伊大学的研究人员通过研究开发并且检测了抗真菌药物两性霉素B的多种衍生物。两性霉素B医生们推出的最后一道抵御真菌感染的防御性药物,该药已经使用了近半个世纪,其被认为可以有效克服新生的耐药性病原体的感染。 研究者Burke表
靶向攻击真菌感染而不损伤人类细胞的新型化合物或许可以有效避免抗生素耐药性的产生;近日,刊登在国际杂志Nature Chemical Biology上的一篇研究论文中,来自伊利诺伊大学的研究人员通过研究开发并且检测了抗真菌药物两性霉素B的多种衍生物。两性霉素B医生们推出的最后一道抵御真菌感染的防御性药物,该药已经使用了近半个世纪,其被认为可以有效克服新生的耐药性病原体的感染。
研究者Burke表示,该药物的主要问题就是毒性较大,尤其是对于肾脏的伤害,因此限制该药的剂量对于治疗病人非常重要;此前研究发现两性霉素B可以通过靶向作用对细菌生理活性重要的脂质分子来杀灭酵母和真菌,但该药物同时也会结合人类机体的胆固醇,从而引发机体毒性。
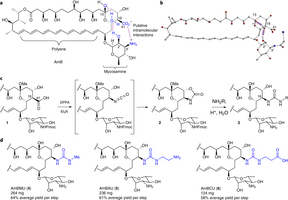
这项研究中,研究者进行了三步简单的化学步骤,将两性霉素B转化成了一种新型化合物,这种化合物可以有效靶向作用真菌的脂质分子,但其并不结合胆固醇分子;随后研究者发现这种特殊衍生物可以抵御小鼠机体的酵母感染,而且对小鼠并不带来任何毒性作用。由于该药物的作用效果较为特殊,因此研究者担心是否会出现耐药性菌株,当对突变的耐药性酵母进行试验后,研究者发现这种衍生物同样也可以对耐药性菌株进行作用。
研究者表示,两性霉素B躲避病原体耐药性的特殊能力或许和其毒性之间存在不寻常的关系,因此他们就推测这些衍生物或许并没有两性霉素B那么容易受到影响,这对于开发新型的抵御耐药性病原体感染的疗法或许非常重要。
研究者希望本文研究可以帮助他们寻找更多可以抵御耐药性真菌感染以及低毒性的化合物,这对于有效杀灭耐药性病原体,同时改善患者的机体健康和生活质量将非常重要。
原始出处:
Stephen A Davis, Benjamin M Vincent, Matthew M Endo, Luke Whitesell, Karen Marchillo, David R Andes, Susan Lindquist & Martin D Burke.Nontoxic antimicrobials that evade drug resistance.Nature Chemical Biology, June 1, 2015.doi:10.1038/nchembio.1821
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#化合物#
0
#Nat#
54
#Biol#
65
#Bio#
60
#抗菌#
53
#病原体#
54