WCLC 2013:EGFR野生型NSCLC二线治疗中培美曲塞优于吉非替尼(CTONG 0806研究)
2013-10-30 MedSci MedSci原创
没有EGFR突变的肺癌患者,靶向药物疗效如何?在悉尼举办的第15届世界肺癌大会上,公布了由吴一龙教授领衔的CTONG 0806研究结果,是今年会议8篇新闻发布论文之一,也是会改变肺癌临床实践的研究。培美曲塞和吉非替尼对于东亚的晚期非鳞非小细胞肺癌患者来讲,都是标准的二线治疗药物。CTONG 0806研究,是一项多中心随机对照开放标签2期试验,目的是探索培美曲塞与吉非替尼作为二线治疗在晚期EGFR野
没有EGFR突变的肺癌患者,靶向药物疗效如何?在悉尼举办的第15届世界肺癌大会上,公布了由吴一龙教授领衔的CTONG 0806研究结果,是今年会议8篇新闻发布论文之一,也是会改变肺癌临床实践的研究。
培美曲塞和吉非替尼对于东亚的晚期非鳞非小细胞肺癌患者来讲,都是标准的二线治疗药物。CTONG 0806研究,是一项多中心随机对照开放标签2期试验,目的是探索培美曲塞与吉非替尼作为二线治疗在晚期EGFR野生型的非鳞非小细胞肺癌的疗效。患者和方法:
纳入局部晚期或转移性非鳞非小细胞肺癌患者,均已经接受过以铂类为基础的化疗治疗,并且直接测序法检测为野生型EGFR。随机分配到接受吉非替尼口服250mg/天(G组)或培美曲塞500 mg/m2,d1,每21天1周期(P组)直至疾病进展或不可耐受的毒性。
研究主要终点是无进展生存期(PFS)。次要终点包括4个月和6个月的PFS率,总生存期(OS),客观缓解率(ORR),疾病控制率(DCR),生活质量和安全性。通过独立审查委员会(IRC)对所有数据进行评估。
研究结果:
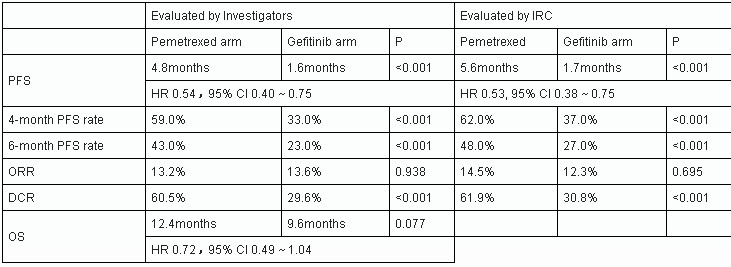
从 2009年2月至2012年8月,共161例患者入选,157例可评估(G组81例,P组76例) 。?基线特征在两组中是平衡的。主要终点中位PFS,在P组为4.8个月,在G组为1.6个月(HR 0.54,95%CI为0.40-0.75,P<0.001),由IRC评测后证实(5.6个月对1.7个月,HR 0.53 ,95%CI为0.38-0.75,P<0.001)。
两个组之间在4个月的PFS率,6个月的PFS率和DCR方面同样体现了显著差异(下表)。中位OS也显示了在P组具有优势的趋势(12.4个月对9.6个月,HR 0.72,95% CI为0.49-1.04,P=0.077)。
G组中出现更多的皮疹和腹泻,而P组更多出现疲劳和ALT升高。CTCAE 3或4级不良事件在G组为12.3 %,在P组为32.9%(P=0.002)。
研究结论:
1、对于晚期EGFR野生型的非小细胞肺癌患者,CTONG0806是第一项显示了二线治疗中,培美曲塞比吉非替尼能够显著改善无进展生存(PFS),疾病控制率(DCR)和存在改善总生存(OS)趋势的研究。
2、二线治疗中,应该明确EGFR突变的状态来指导临床治疗。相比直接测序方法,ARMS能够更好的确定哪些患者能从EGRF-TKI治疗中获益。
3、对于EGFR野生型的晚期非小细胞肺癌患者,二线治疗应该推荐使用疗效和耐受性均更好的培美曲塞。
MedSci一句话短评:
本研究结果与此前公布的TAILOR研究类似(Lancet Oncol:EGFR野生型NSCLC二线治疗:厄洛替尼不敌标准化疗(TAILOR研究)),靶向治疗必需“认靶”!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#野生型#
43
#美曲塞#
49
#CTO#
66
#培美曲塞#
62
#WCLC#
51
#GFR#
62
#二线治疗#
51