


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





新型自膨式可复位的经导管心脏瓣膜(THV)系统是被设计用于治疗严重的有临床症状且外科风险的主动脉瓣狭窄患者。本研究的目的旨在评估该新型THV系统的1年疗效。本次多中心临床试验是用于评估植入该新型THV后30天、1年和5年的预后,主要终点事件是术后1年的全因死亡率,次要终点事件是临床预后和心超指标。最终共纳入941名患者(82.4 ± 5.9岁,女性占65.7%),术后1年,全因死亡率、心血管死亡率
经导管主动脉瓣置换术(ViV-TAVR)是切实可行的,然而其安全性与有效性和自体瓣膜TAVR(NV-TAVR)相比如何尚不清楚。本研究的目的旨在评估ViV-TAVR在外科主动脉瓣置换术(SAVR)失败患者中的安全性和有效性,并与NV-TAVR进行比较。本研究纳入了1150名接受ViV-TAVR治疗的患者,并1:2匹配了2259名接受NV-TAVR治疗的患者。非调整分析结果显示,与NV-TAVR患者
使用爱德华兹Sapien THV的经导管肺动脉瓣置换术在3年的随访中表现出优秀的瓣膜功能和临床结局。
经导管主动脉瓣置换术在低外科风险的严重主动脉瓣狭窄患者中安全有效,并发症更低,住院时间更短,30天死亡率为零。
本研究的目的旨在比较和评估美国关键高风险CoreValve 临床试验中经导管主动脉瓣置换术(TAVR)和外科主动脉瓣置换术(SAVR)的5年预后。本次临床试验将外科高风险患者随机1:1分至自膨式TAVR组和SAVR组,严重血流动力学结构瓣膜恶化定义为平均跨瓣压差 ≥40 mm Hg或压差改变≥20 mm Hg或新发的严重主动脉瓣反流。最终纳入了来自45个美国医疗中心的750名手术患者(TAVR =
经股经导管主动脉瓣置换术(TF-TAVR)在治疗主动脉瓣狭窄中的应用越来越广泛,但其术后的卒中发生风险尚不清楚。本研究的目的旨在比较和评估外科主动脉瓣置换术(SAVR)和TF-TAVR术后的生活质量与卒中发生的关系。本研究纳入了PARTNER 临床研究中的1204对因严重主动脉瓣狭窄接受SAVR和TF-TAVR治疗的患者,临床结局是:1. 30天的神经病学事件;2. 术后早期(≤7天)和晚期(7天


梅斯医学MedSci APP
医路相伴,成就大医
厉害厉害,必须点赞
118
#主动脉#
72
#动脉夹层#
72
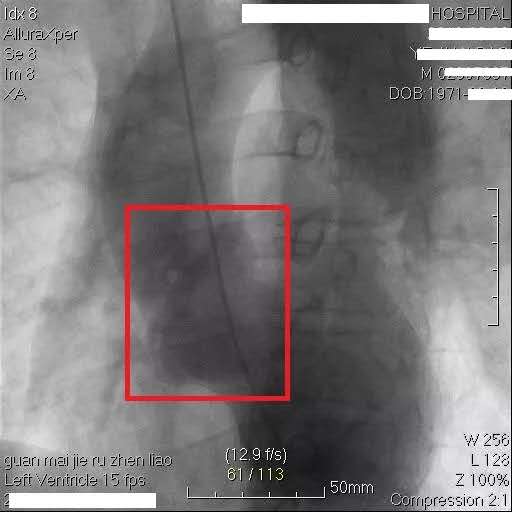
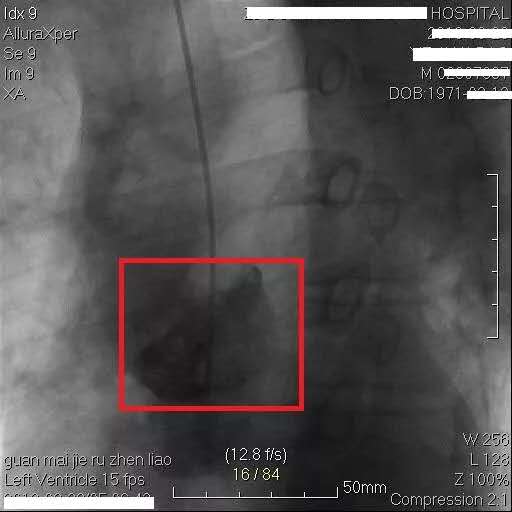
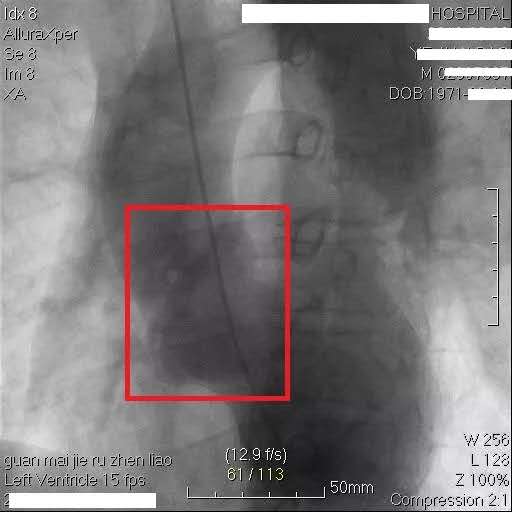
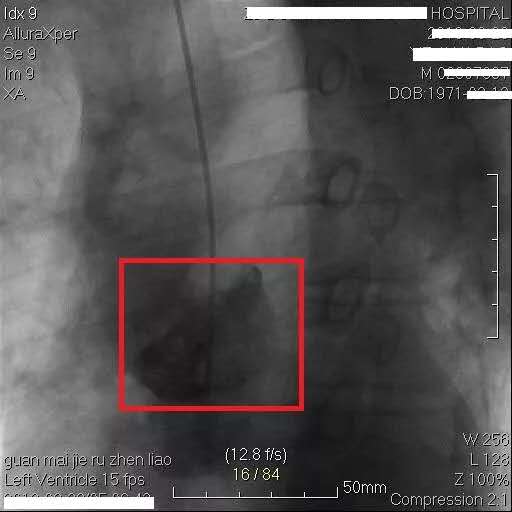
导管捅出主动脉夹层。
99
引以为戒引以为戒!
105