PLOS Biology:研究发现脑修复的潜在药物
2017-04-02 佚名 生物谷
苏黎世大学的Kasum Azim及其来自里昂大学和朴茨茅斯大学的同事发现了一种新药可以激活小鼠脑部干细胞发育成成熟脑细胞,这项研究于近日发表在PLOS BIOLOGY 上。这项发现也许开启了治疗退行性脑疾病的新药研发新途径。
苏黎世大学的Kasum Azim及其来自里昂大学和朴茨茅斯大学的同事发现了一种新药可以激活小鼠脑部干细胞发育成成熟脑细胞,这项研究于近日发表在PLOS BIOLOGY 上。这项发现也许开启了治疗退行性脑疾病的新药研发新途径。
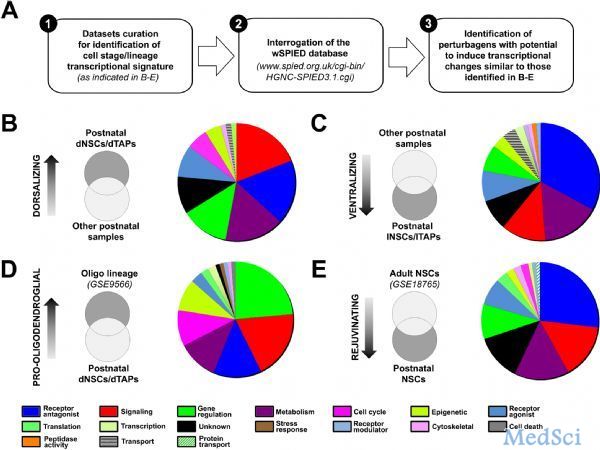
整个成年期,来自脑室下区的神经干细胞都会发育成新神经和支持细胞——小突胶质细胞。新生小鼠各种细胞发育相关的转录改变在公共数据库中进行了分类,类似,被批准用于临床的各种化学物质引起的转录改变也被进行了分类。在这项新研究中,作者使用这些数据库发现细胞分化和药物治疗引起的转录改变发生了重叠,这意味着这些药物可能是逆转神经退行性疾病的潜在药物。
为此,他们研究了脑室下区各种微区的信号通路的差别,结果发现神经特异性微区和少突胶质细胞微区信号通路之间有几个重要的差别,他们就使用这些发现在小分子药物数据库中筛查相似的基因表达水平改变。
结果,他们找到了一系列具有相似转录信号的小分子药物。其中一种叫做LY-294002,可以特异性促进新生小鼠神经干细胞生成正常的小突胶质细胞。成年小鼠体内,不同的分子(AR-A014418和CHIR99021)可以消除成年人脑室下区神经源性能力和细胞多样性的消失。最终发现后者在围产期缺氧脑损伤模型中具有强烈的促进小突胶质细胞再生的能力,及轻微增加神经元数量的能力。
这些结果可以以以下几种方式发挥作用:1)由于小分子药物数据库指出了重要的细胞通路,因此他们为神经发育和修复机理提供了新观点,这可以用于探索新的治疗策略。2)他们发现了几种已经被批准用于临床的新药,现在可以探索这些药物在修复脑损伤中的潜在作用。3)他们提供了一种发现可直接影响神经再生、可能用于治疗脑部疾病的药物的概念性新方法。
“控制神经干细胞的命运是再生医学的关键治疗策略。”Azim及其同事说道,“我们的研究所示的策略允许我们快速鉴定多种药物候选物,并将它们纳入药物开发生产线,它们的治疗潜力可以被进一步评估。”
原始出处:
Kasum Azim, Diane Angonin, Guillaume Marcy et al. Pharmacogenomic identification of small molecules for lineage specific manipulation of subventricular zone germinal activity. PLOS Biology, 2017; 15 (3): e2000698 DOI: 10.1371/journal.pbio.2000698
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#潜在药物#
61
#研究发现#
41
#Biol#
46
#Bio#
52