Cell:HIF-1在缺氧中调节的新靶点!
2017-04-09 MedSci MedSci原创
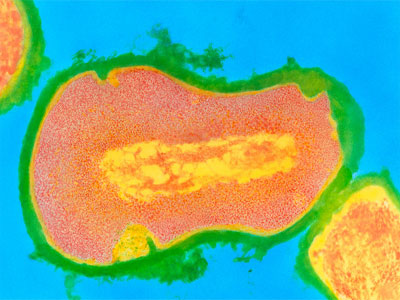
缺氧不仅影响发育,也是许多人类疾病的病理性刺激。细胞水平上对缺氧的反应依赖于转录因子家族的缺氧诱导因子(HIF)的活性。HIF-1负责急性反应并涉及细胞代谢、细胞死亡和细胞生长的各种基因。近期,一项发表在权威杂志Cells上的研究显示了缺氧导致人赖氨酸(K)特异性脱甲基酶2(KDM2)家族的成员KDM2A和KDM2B以及黑腹果蝇KDM2组蛋白和蛋白脱甲基酶的mRNA水平的增加。在人类细胞中,KDM
缺氧不仅影响发育,也是许多人类疾病的病理性刺激。
细胞水平上对缺氧的反应依赖于转录因子家族的缺氧诱导因子(HIF)的活性。HIF-1负责急性反应并涉及细胞代谢、细胞死亡和细胞生长的各种基因。
近期,一项发表在权威杂志Cells上的研究显示了缺氧导致人赖氨酸(K)特异性脱甲基酶2(KDM2)家族的成员KDM2A和KDM2B以及黑腹果蝇KDM2组蛋白和蛋白脱甲基酶的mRNA水平的增加。
在人类细胞中,KDM2家族成员的mRNA水平在缺氧条件下受HIF-1而不是HIF-2的调节。有趣的是,只有KDM2A蛋白水平以HIF-1依赖性的方式显着诱导,而KDM2B蛋白以细胞类型依赖性方式改变。
重要的是,此项研究证明在人类细胞中,缺氧和HIF-1调节KDM2A的过程发生在启动子水平,HIF-1与RNA聚合酶II募集所需的KDM2A启动子结合。
此项研究结果表明,KDM2是一种新颖的HIF靶点,可以帮助协调细胞对缺氧的反应。此外,这些结果也可能解释了为什么KDM2水平通常在人类癌症中失控。
原始出处:
Batie M, Druker J, et al. KDM2 Family Members are Regulated by HIF-1 in Hypoxia. Cells. 2017 Mar 17;6(1). pii: E8. doi: 10.3390/cells6010008.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
79
#Cell#
84
#新靶点#
67
#HIF#
58
cells,notCell.
111
新的发现了。
119