Nature Commun:靶向细胞骨架抑制肿瘤转移新发现
2015-06-23 佚名 生物谷
近日,来自美国的华人科学家在国际学术期刊nature communication在线发表了一项最新研究进展,他们利用高通量筛选的方法发现了一些小分子能够特异性靶向参与肌动蛋白组装的关键蛋白--Fascin,同时证明抑制Fascin的活性能够阻断丝状伪足形成,抑制肿瘤的迁移和侵袭。 肿瘤转移的一个关键步骤是肿瘤细胞的迁移和侵袭,这一过程的实现需要细胞内细胞骨架蛋白的重新排列。丝状伪足是参与肌动蛋白
近日,来自美国的华人科学家在国际学术期刊nature communication在线发表了一项最新研究进展,他们利用高通量筛选的方法发现了一些小分子能够特异性靶向参与肌动蛋白组装的关键蛋白--Fascin,同时证明抑制Fascin的活性能够阻断丝状伪足形成,抑制肿瘤的迁移和侵袭。
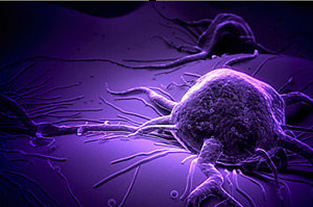
肿瘤转移的一个关键步骤是肿瘤细胞的迁移和侵袭,这一过程的实现需要细胞内细胞骨架蛋白的重新排列。丝状伪足是参与肌动蛋白细胞骨架突起形成的一种重要结构,其作用相当于细胞的感受器官,能够与细胞外微环境进行信息交流,同时还参与一些基础的细胞功能如细胞黏附,扩展以及在三维环境中迁移。
之前一些研究已经发现丝状伪足在肿瘤细胞侵袭的起始阶段可能发挥主要作用,癌细胞可利用丝状伪足向器官表面粘附和侵袭,而Fascin是丝状伪足形成过程中参与肌动蛋白组装的一个重要蛋白,因此研究人员认为靶向Fascin开发小分子药物或许是抑制癌症转移的一种潜在方法。
在该项研究中,研究人员利用高通量筛选的方法,发现了一些小分子能够抑制Fascin的肌动蛋白组装活性,随后,研究人员将目光集中在其中一个小分子抑制剂上,证明这种小分子抑制剂能够特异性阻断丝状伪足的形成,进而抑制肿瘤细胞在体外的迁移和侵袭,以及肿瘤细胞在体内的转移。
在对实验结果进行充分验证和分析之后,研究人员认为具有靶向特性的Fascin抑制剂可能对于癌症治疗具有潜在治疗效果,这项研究对于转移性癌症的治疗具有一定意义。
原始出处:
Fang-Ke Huang, Shaoqin Han, Bowen Xing, Jianyun Huang, Bingqian Liu, Francois Bordeleau, Cynthia A. Reinhart-King, J. Jillian Zhang & Xin-Yun Huang.Targeted inhibition of fascin function blocks tumour invasion and metastatic colonization.Nature Commuications, June 17, 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#COMMUN#
60
#抑制肿瘤#
65
#Nat#
51
#新发现#
63
#靶向细胞#
69
看看
148
#肿瘤转移#
55
细胞骨架应该能成为抗肿瘤的靶点
182