Nat Commun:血浆ctDNA可作为肿瘤组织的代用品来实现转移性膀胱癌的临床基因组分层
2021-01-30 AlexYang MedSci原创
分子分层可以改善晚期癌症的治疗,但需要相关的肿瘤样本。转移性尿道癌(mUC)将受益鉴于最近治疗方案的扩展及其高基因组异质性。
分子分层可以改善晚期癌症的治疗,但需要相关的肿瘤样本。转移性尿道癌(mUC)将受益鉴于最近治疗方案的扩展及其高基因组异质性。
最近,有研究人员对104名mUC患者的微创血浆循环肿瘤DNA(ctDNA)样本进行了解析,并与侵入性手术期间获得的相同患者肿瘤组织进行了比较。研究发现,患者ctDNA丰度对起始使用一线系统治疗的患者的总生存率具有独立的预后。重要的是,ctDNA分析重现了基于组织队列描述的体细胞驱动基因组。此外,ctDNA和匹配的肿瘤组织之间的突变一致性为83.4%,使得拟议的临床生物标志物能够实现基准化。虽然90%的突变在ctDNA样本中能够识别出来,但肿瘤组织的一致性明显较低。
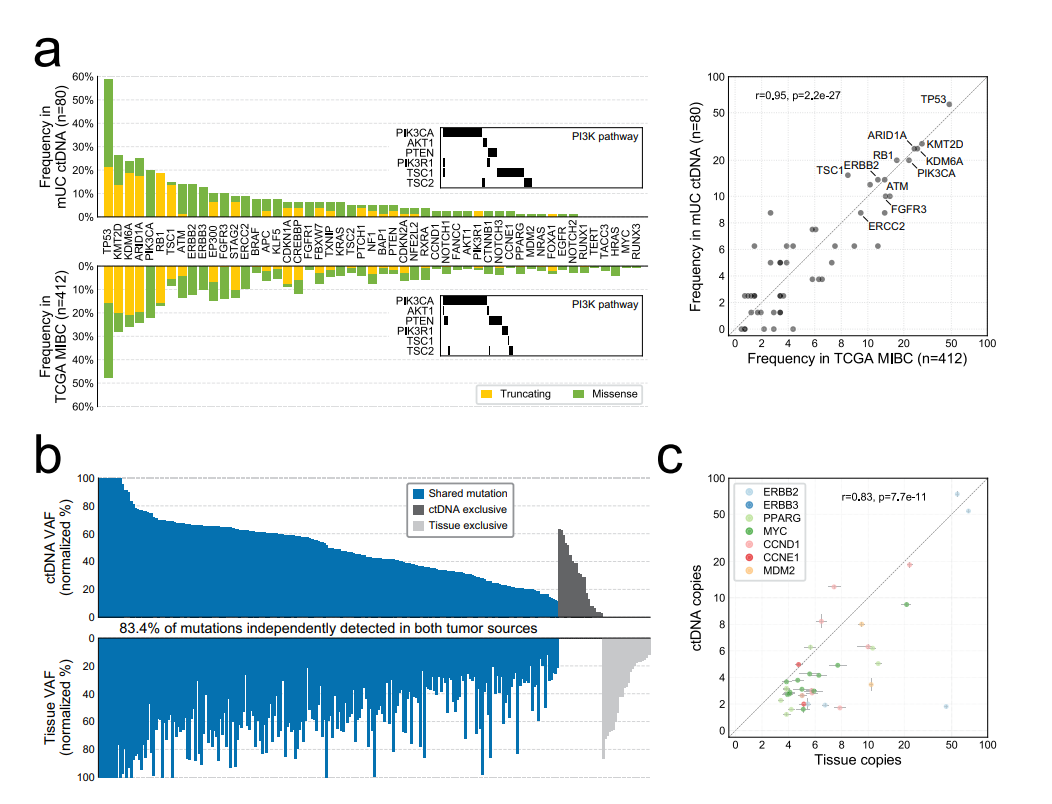
CtNDA与肿瘤组织的比较
最后,研究人员指出,mUC中ctDNA的基因组图谱是可靠和实用的,弱化了原发肿瘤灶所固有的疾病采样不足。因此,研究人员推荐将无细胞DNA解析纳入mUC的分子指导临床试验中。
原始出处:
Gillian Vandekerkhove, Jean-Michel Lavoie, Matti Annala et al. Plasma ctDNA is a tumor tissue surrogate and enables clinical-genomic stratification of metastatic bladder cancer. Nat Commun. Jan 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
58
#COMMUN#
64
高校博士科研团队,提供SCI论文科研服务,文章提供原始数据,作者审核文章内容及结果后投稿,可指定拟投杂志,文章接受后付款,前期不收任何费用。术业有专攻,期待与您的合作1615858451
113
学习
108
#转移性#
57
#肿瘤#
147
膀胱癌真怪,明明是免疫敏感性肿瘤,为什么PD-1治疗效果不好呢?难道靶点不对?将来CD47会不会有效
69