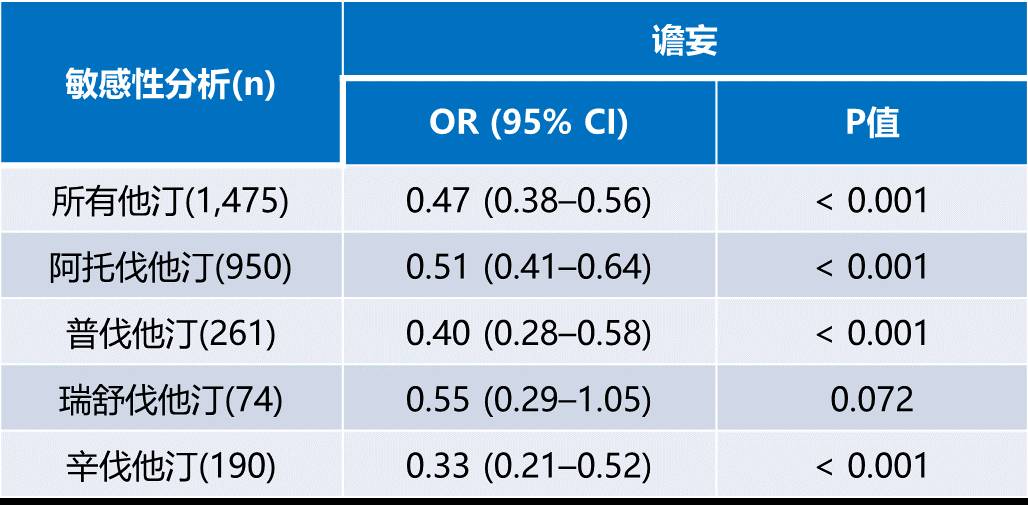
JAMA:预防性氟哌啶醇对谵妄高风险危重病患者的疗效
2018-03-09 杨中华 脑血管病及重症文献导读
谵妄是一种急性脑病,特征为急性发作的意识模糊,注意力不集中和意识水平变化,这些症状在一天之中波动。ICU中谵妄非常常见,发生率为30-50%。谵妄与临床预后不良有关,包括机械通气时间延长,增加ICU和住院时间,增加死亡率。并且,当谵妄消失后,认知功能损害将持续。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#高风险#
61
#危重病#
75
#预防性#
57
学习了提高了
100
学习了.谢谢分享
90
#氟哌啶醇#
0
学习谢谢分享
110
学习了.涨知识
96
了解了解.继续关注
90
好好好学习天天向上
43