Science:小心了!这两种肠道细菌一碰头,就可能引发结肠癌!
2018-02-03 佚名 学术经纬
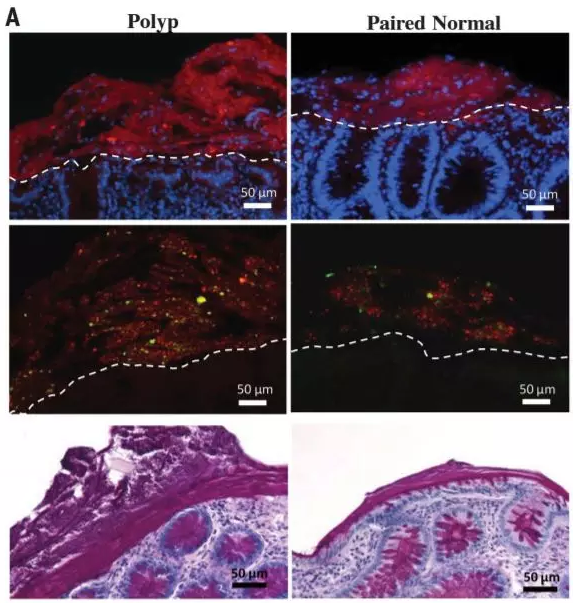
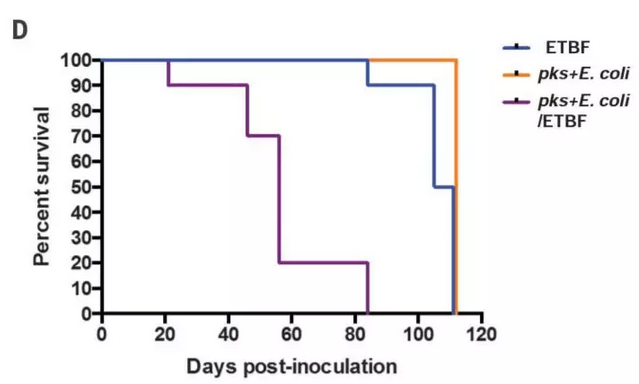
在最新一期的《科学》上,约翰·霍普金斯大学医学院 Cynthia Sears 教授带领的团队报道了肠道菌群如何参与结肠癌的发生与发展:研究发现脆弱拟杆菌(Bacteroides fragilis)和一种大肠杆菌(psk+ Escherichia coli)两种肠道菌群会联手形成生物膜,损坏结肠粘膜,引发结肠癌。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












非常好
94
学习一下谢谢分享
102
#肠道细菌#
53
#SCIE#
47
学习了
89
学习啦.很好的文章
100
学习了
94
不错的文章值得拥有
53
不错的文章值得拥有
68
了解了解.继续关注
68