Blood:囊胚和多形性套细胞淋巴瘤的诊断和治疗!
2018-11-02 MedSci MedSci原创
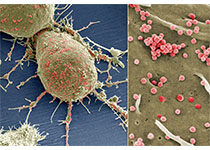
囊胚套细胞淋巴瘤的特点是具有高度侵袭性,临床病程短。胚泡和多形性变异可通过细胞形态学特征进行定义,但标准多少存在主观性。根据Ki-67标记指示的细胞高度增殖或可支持诊断。但近期分析表明Ki-67指数推翻了从细胞学亚型衍生的预后。遗传学分析表明胚泡和多形性突变体与典型套细胞淋巴瘤明显不同。在临床队列中,该亚型发病率的浮动很大,大概占全部病例的10%。通常用于套细胞淋巴瘤的化疗方案,如苯达莫司汀,以标
囊胚套细胞淋巴瘤的特点是具有高度侵袭性,临床病程短。胚泡和多形性变异可通过细胞形态学特征进行定义,但标准多少存在主观性。根据Ki-67标记指示的细胞高度增殖或可支持诊断。但近期分析表明Ki-67指数推翻了从细胞学亚型衍生的预后。
通常用于套细胞淋巴瘤的化疗方案,如苯达莫司汀,以标准剂量治疗经典突变型套细胞淋巴瘤(如囊胚套细胞淋巴瘤),很少能延长其缓解期。因此,根据这类患者高度侵袭性的临床病程,一般推荐采用包含大剂量阿糖胞苷的化疗方案,并配以大剂量的巩固治疗。
但是,即使采用强化治疗方案,这类患者的长期预后仍不乐观。因此,或许应在该疾病患者的病程早期即考虑采用异基因移植。此外,靶向治疗在该类患者中也是迫切需要的,但相关临床数据匮乏。依鲁替尼治疗可获得较高的缓解率,但缓解持续时间(中位值)短于6个月。与之类似,来那度胺和西罗莫司治疗也仅可获得短期缓解。
像CAR-T细胞这样的新疗法或许可最终改善这类患者的长期预后。
原始出处:
Martin Dreyling, Wolfram Klapper, and Simon Rule. Blastoid and pleomorphic mantle cell lymphoma: still a diagnostic and therapeutic challenge. Blood 2018 :blood-2017-08-737502; doi: https://doi.org/10.1182/blood-2017-08-737502
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞淋巴瘤#
61
#多形性#
77
啦啦啦啦啦啦啦啦啦啦啦啦啦啦
93
谢谢了,学习
113
学习学习学习
81
学习了
71