JACC:症状出现超过12小时的STEMI患者仍能从血运重建中明显获益!
2021-10-05 Nebula MedSci原创
冠状动脉血管重建可显著改善症状出现超过12小时的STEMI患者的短期和长期临床预后
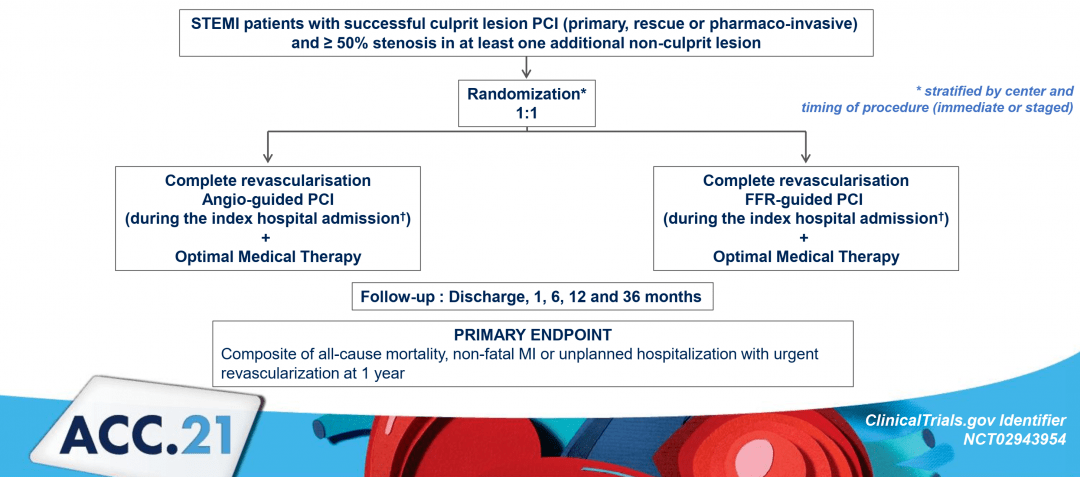
毋庸置疑,急性心肌梗死患者越早恢复心肌血流灌注的预后越好。但是,临床上有大量的ST段抬高型心肌梗死(STEMI)患者因各种原因就诊时距症状出现已超过12小时,据多项临床研究(GRACE、TETAMI)统计,这类患者占了所有因急性心肌梗死就诊患者的12-40%。迄今为止,症状出现超过12小时的STEMI患者的最佳治疗方案仍未有定论。
本研究目的是在大量晚期STEMI患者中总结这类患者的特征、时间趋势,以及血运重建对其预后的意义。
研究人员分析了来自FAST-MI项目的三项国家性观察研究的数据(2005年、2010年和2015年)。晚期STEMI定义:就诊时距离症状出现12-48小时。
有无血运重建的患者的全因死亡率
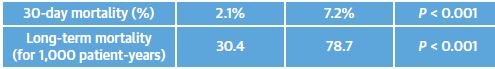
从3个队列中共纳入了6273位STEMI患者,其中1169位(18.6%)为晚期STEMI。排除接受纤溶治疗的和入院后2天内死亡的患者,最终分析纳入了1077位患者,其中729位(67.7%)在入院后48小时内进行了血运重建。随访30天时,进行了血运重建的晚期STEMI患者的全因死亡率明显降低(2.1% vs 7.2%; p<0.001)。中位随访了58个月后,血运重建组晚期STEMI患者的全因死亡率为30.4/1000人·年(95% CI 25.7-35.9),而未接受血运重建的晚期STEMI患者的全因死亡率为78.7/1000人·年 (95% CI 67.2-92.3;p<0.001)。
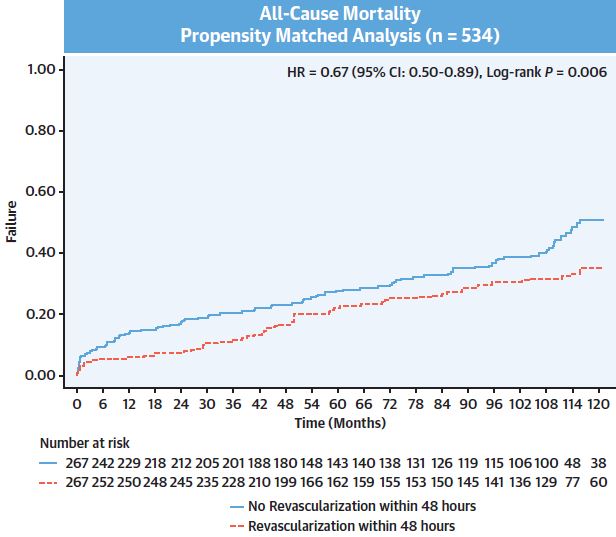
有无血运重建的患者的全因死亡率
在多变量分析中,晚期STEMI患者血运重建与随访过程中的死亡率显著降低独立相关(HR 0.65 [95% CI 0.50-0.84]; p=0.001)。
总而言之,虽然晚期STEMI患者已错过最佳血运重建时间(症状出现后12小时内),但接受冠状动脉血管重建仍能明显改善其短期和长期临床预后。
原始出处:
Bouisset Frédéric,Gerbaud Edouard,Bataille Vincent et al. Percutaneous Myocardial Revascularization in Late-Presenting Patients With STEMI.[J] .J Am Coll Cardiol, 2021, 78: 1291-1305. https://doi.org/10.1016/j.jacc.2021.07.039
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#STEMI患者#
90
#JACC#
81
学习
99
#ACC#
95
#STEM#
106
认真学习了
87
学习了,谢谢
97
学习了👍
91
好文章,谢谢分享。
102