内分泌联合放疗是高危局限性前列腺癌的更佳治疗
2015-03-03 CMT 中国医学论坛报
放疗+内分泌治疗优于单独内分泌治疗 美国国立综合癌症网络(NCCN)将局限性前列腺癌(T3a)、或Gleason评分为8~10分、或PSA≥20 ng/ml列为高危患者,这些患者的标准治疗方案是手术或根治性外照射放疗(EBRT)联合内分泌去势治疗。 欧洲癌症研究与治疗组织(EORTC)一项临床研究评估了接受外照射放疗的高危前列腺癌患者接受长期去势内分泌治疗的获益情况。共入组415例
放疗+内分泌治疗优于单独内分泌治疗
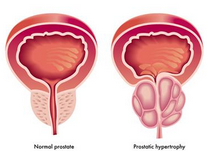
美国国立综合癌症网络(NCCN)将局限性前列腺癌(T3a)、或Gleason评分为8~10分、或PSA≥20 ng/ml列为高危患者,这些患者的标准治疗方案是手术或根治性外照射放疗(EBRT)联合内分泌去势治疗。
欧洲癌症研究与治疗组织(EORTC)一项临床研究评估了接受外照射放疗的高危前列腺癌患者接受长期去势内分泌治疗的获益情况。共入组415例患者,随机接受放疗联合3年去势内分泌治疗或单独放疗,结果显示,放疗联合内分泌治疗显著提高了患者的10年生存率(58.1% 对 39.8%,P=0.004)。与之类似的其他研究获得了同样的结论。
对于高危局限性前列腺癌,放疗联合内分泌治疗是否优于单纯去势内分泌治疗,同样有一系列前瞻性及回顾性研究对此进行了评估。一项入组了875例的随机Ⅲ期临床研究显示,与单独内分泌治疗比较,内分泌治疗联合放疗可以使10年前列腺癌特异性死亡率降低一半(11.9%对23.9%)。另外一项纳入15170例患者的回顾性队列研究发现,单纯内分泌治疗并不适合高危局限性前列腺癌,目前也无任何指南或循证医学证据支持单纯去势内分泌治疗用于高危局限性前列腺癌的治疗。
因此,对于高危局限性前列腺癌患者,放疗联合去势内分泌治疗是最佳的治疗选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#联合放疗#
106
很不错学习了
133
#分泌#
60
#局限性#
69
#局限性前列腺癌#
82