SPRINT研究的启示:优化方案,联合降压,尽早达标
2015-12-29 中国医学科学院阜外心血管病医院 党爱民 中国医学论坛报
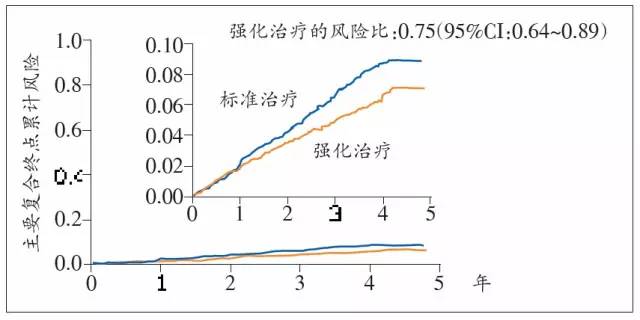
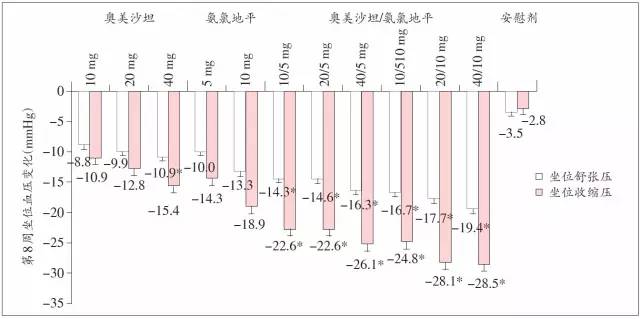
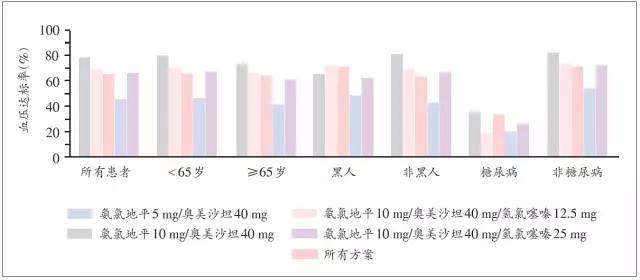
SPRINT研究因强化降压组获益显著而被提前终止,并在2015美国心脏学会(AHA)科学年会上公布研究细节,高血压患者的降压目标值问题再次引发了国内外心血管界广泛的关注和讨论。尽管该研究中的强化降压目标(SBP<120 mmHg)并非适用于所有伴有危险因素的高血压患者,而尚不能作为降压目标被新的指南所推荐,但强化降压显著降低心血管事件和全因死亡风险的理念被再次夯实,并将对未来高血压指南的制订和更新
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SPRINT#
73
#SPRINT研究#
63
联合降压不错,
99
联合降压不错,
126
联合降压是个不错的方式,
95
联合降压是个不错的方式,
125
嗯…
166
好文章
159
好文章
119
值得分享,谢谢分享,
96