Nature子刊:生物3D打印再升级,重塑人耳!
2016-12-27 生物探索 生物探索
导读 2月15日,Nature子刊《Nature Biotechnology》在线发表一篇文章,揭示了一种最新的生物3D打印技术ITOP 。通过使用新型生物材料,该打印技术能够构建出结构稳定且具备功能的人耳器官、骨骼和肌肉组织,更重要的是这些组织器官微通道,能够维持其继续生长形成血管、软骨等系统,从而发挥功能。
导读 2月15日,Nature子刊Nature Biotechnology(IF:43.113)在线发表一篇文章,揭示了一种最新的生物3D打印技术ITOP 。通过使用新型生物材料,该打印技术能够构建出结构稳定且具备功能的人耳器官、骨骼和肌肉组织,更重要的是这些组织器官微通道,能够维持其继续生长形成血管、软骨等系统,从而发挥功能。
从材料学、航空领域、工业器械到生物行业,3D打印技术正以热门、创新的姿态渗入其中。同时,生物3D打印是再生医学、器官移植领域不可忽视的一种新兴力量。不少实验室都将生物3D技术构建组织、器官作为研究课题,致力于突破组织工程学的局限和难题。
作为再生医学的热门“利器”,目前的三维打印技术虽然实现了组织、器官的构建,但是还不能研发出足够完整、强度的功能性组织结构,用于人体一直。
2月15日,Nature子刊《Nature Biotechnology》在线发表一篇文章,揭示了一种最新的3D打印技术——Integrated Tissue and Organ Printing (ITOP) 。通过使用新型生物材料,该打印技术能够构建出结构稳定且具备功能的人耳器官、骨骼和肌肉组织,更重要的是这些组织器官融入微通道,能够维持其继续生长形成血管、软骨等系统,从而发挥功能。
ITOP融入微通道,构建出人耳、骨肉、肌肉等组织结构
ITOP技术由来自于维克森林大学浸信医学中心(WFUBMC)再生医学系主任Anthony Atala研究团队历经十年之久研发而成。
ITOP技术原理:利用类似于塑料的可降解生物材料和优化的水性凝胶,结合3D打印技术实现组织结构的重建,且这些材料能够支撑整个结构,保证细胞包含其间不受到损伤。特别注意的是,凝胶包含了微通道(micro-channels),能够与身体构建连接,实现氧气、营养等物质的运输,为细胞的生长提供环境,从而实现其功能。
ITOP技术已有成果:Atala团队构建了小型人耳器官,并将其移植至老鼠身上。观察2个月后,实验小鼠身体上的耳朵依旧保持原有结构,且已经形成软骨组织和血管系统。
这一试验结果表明,通过结合生物学原理融入微通道,能够为细胞提供各必需营养物质,支持细胞和组织的生长和功能。这些微通道为打印组织的血管、神经系统形成提供了可能。
研究人员使用ITOP系统和人类干细胞构建下颌骨碎片,用于人面部重建和修复。试验中,研究人员将下颌骨碎片移植至老鼠身上。5个月后,这些骨头碎片已经形成血管。
此外,研究人员也成功构建出肌肉组织,并植入老鼠模型。这类新技术构建的组织、器官都能够生成血管、神经系统 在2周内,且其本身形状并不改变。
有望实现个性化再生医学
Atala团队认为,既然ITOP技术能够实现细胞生长、维持组织结构功能,那么它将能够应用于个性化的再生医学领域
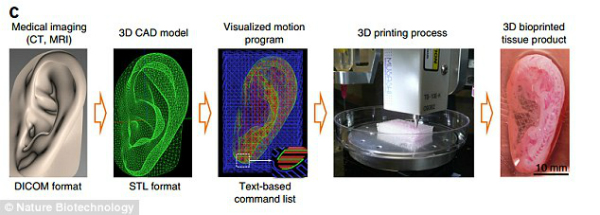
他们设想,通过CT、核磁共振成像等技术获取不同患者的身体结构数据,结合打印软件分析,构建匹配的3D式组织和器官。随着技术的进步,ITOP将有望实现个性化组织器官重建,用于手术移植等过程。
原始出处:
[1] Honor Whiteman. Functional human body parts built using 3D-bioprinting technique. MNT.16 February 2016.
[2] Victoria Woollaston . 'Fifth Element 3D printer' creates first human ear with blood vessels in breakthrough that paves the way for printable body parts. MailOnline. 15 February 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







对.最重要的是3D打印的器官要能够在患者身上生长
94
#Nat#
50
#3D#
50
很有价值
110
好厉害哦!你说过了
102