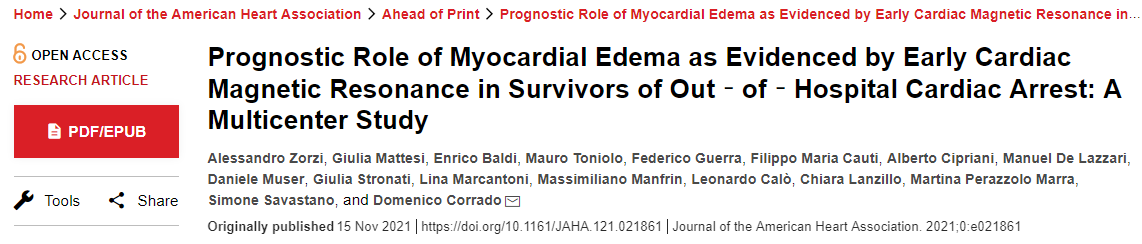
JAHA:院外心脏骤停幸存者早期心脏磁共振查出心肌水肿的预后作用
2021-11-16 MedSci原创 MedSci原创
早期心脏磁共振成像的ME表明急性和短暂的致心律失常基质,预测SCA幸存者的长期心律失常结局良好。这些结果可能会对未来SCA幸存者治疗指南产生重大的影响。
心脏骤停(SCA)可能由急性和可逆的心肌损伤、慢性和不可逆的心肌损伤或原发性室性心律失常所引起。心脏磁共振成像可以识别心肌水肿(ME),它提示急性和可逆性的心肌损伤。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员在随访期间评估了SCA幸存者的心律失常结局,并进一步评估了ME的预后作用。
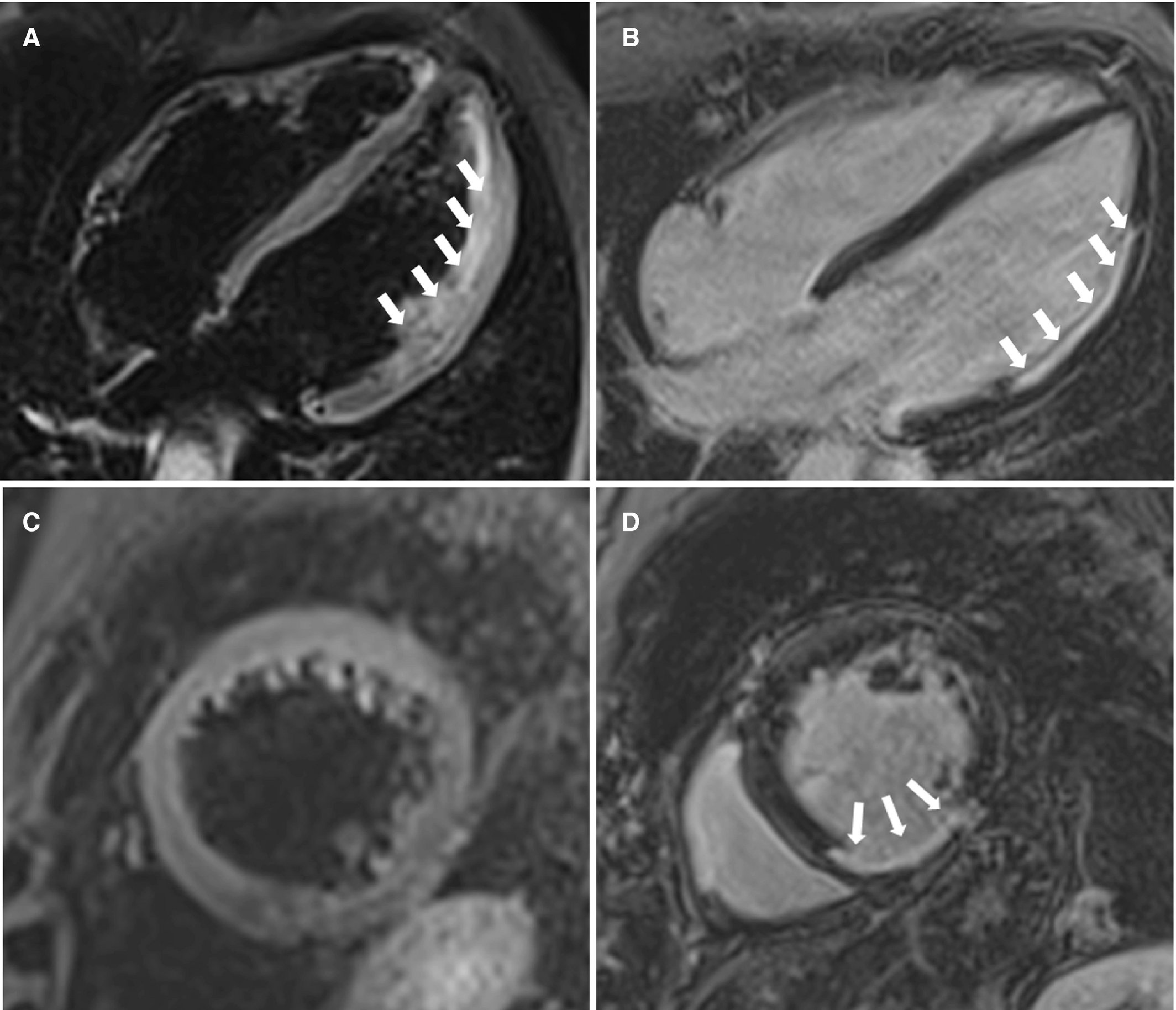
研究人员连续纳入了来自9个合作中心的101名(71%为男性,中位年龄为47岁)SCA幸存者,他们接受了早期(<1个月)心脏磁共振成像检查并接受了植入式心脏复律除颤器(ICD)。在T2加权序列中,101名患者中有18名(18%)患者发现了ME。根据心脏磁共振成像检查结果,心律失常性SCA归因于急性心肌损伤(缺血性[n=10]或炎症性[n=8])、慢性结构性心脏病(缺血性心脏病[n=11]、心肌病)[n=20],或其他[n=23])或主要为心律失常综合征(n=29)。
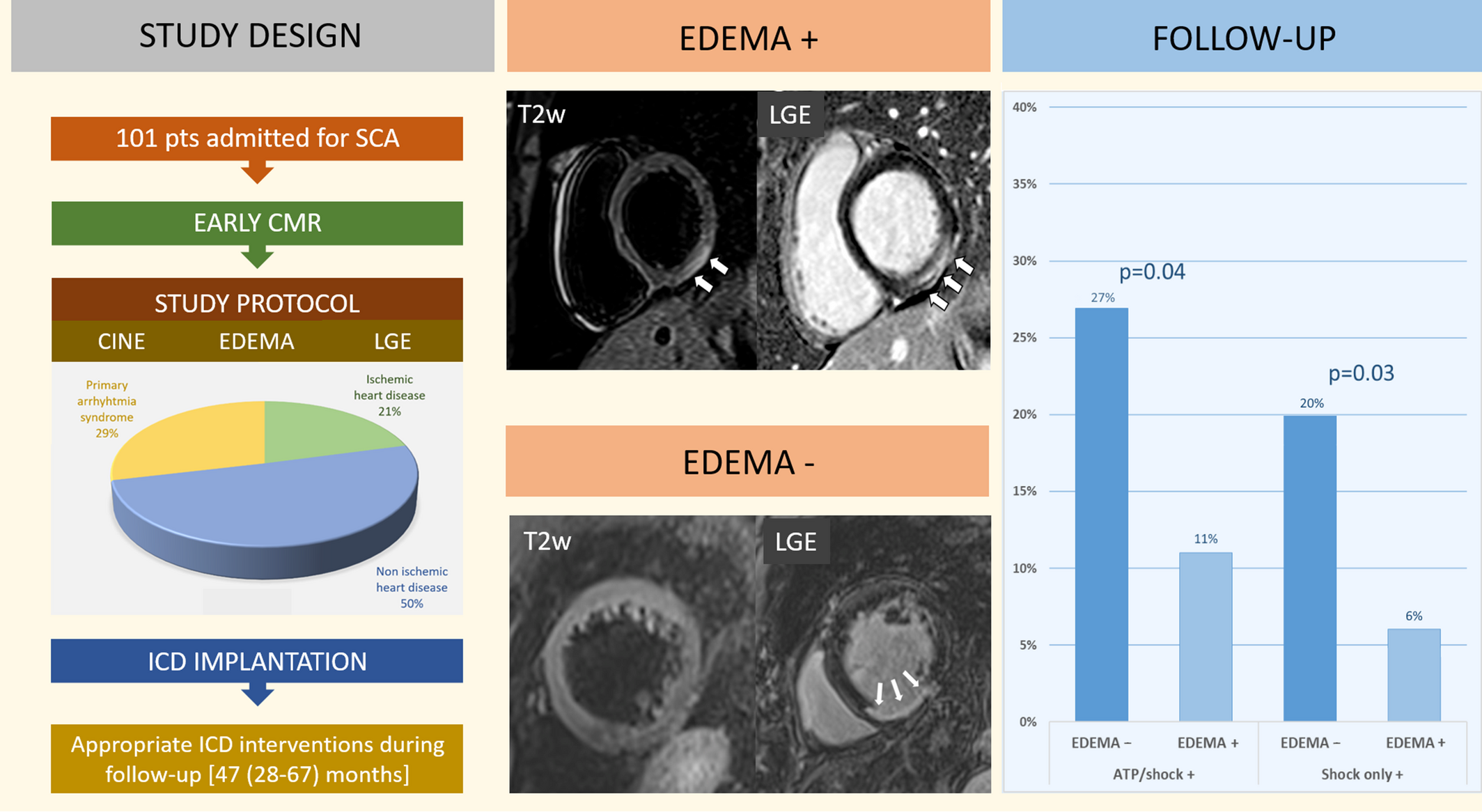
在47个月(28至67个月)的随访期间,101名患者中有24名(24%)患者接受了适当的ICD干预治疗。ME与无任何ICD干预(log-rank=0.04)和ICD电击(log-rank=0.03)的显著更高的生存率相关,并且在调整左心室射血分数和晚期钆增强后仍然是更好的心律失常结局的独立预测因子。适当的ICD干预的风险与潜在心脏病的类型无关。
由此可见,早期心脏磁共振成像的ME表明急性和短暂的致心律失常基质,预测SCA幸存者的长期心律失常结局良好。这些结果可能会对未来SCA幸存者治疗指南产生重大的影响。
原始出处:
Alessandro Zorzi,et al.Prognostic Role of Myocardial Edema as Evidenced by Early Cardiac Magnetic Resonance in Survivors of Out‐of‐Hospital Cardiac Arrest: A Multicenter Study.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.021861
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AHA#
78
#院外心脏骤停#
73
#水肿#
0
#磁共振#
67
#心脏磁共振#
68