【所属科室】
肿瘤科
【基本资料】
女性,56岁
【主诉】
腹胀2月余,发现腹盆腔包块1天
【查体】
腹膨隆,扪及24x24x15cm肿块,呈囊性,边界清,上界达剑突下,活动可,无压痛
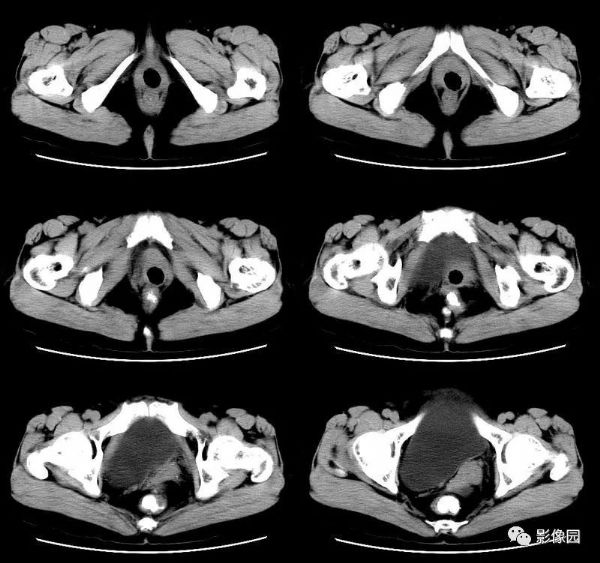
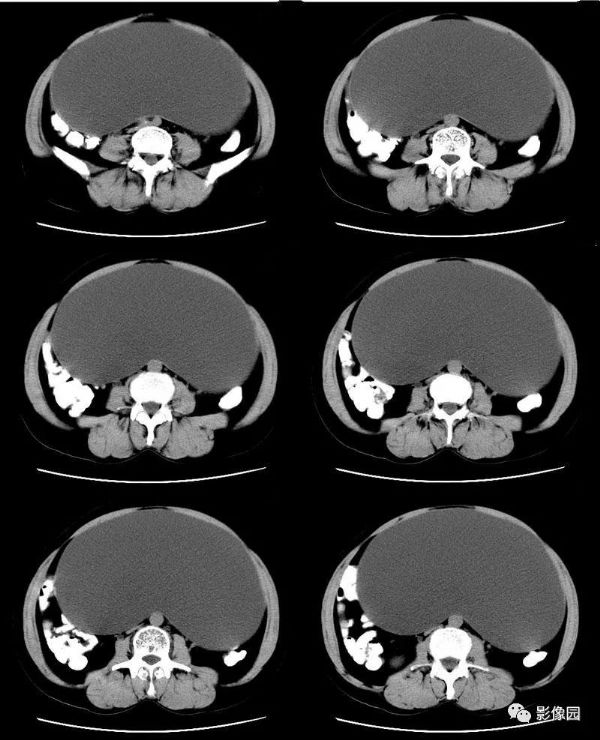
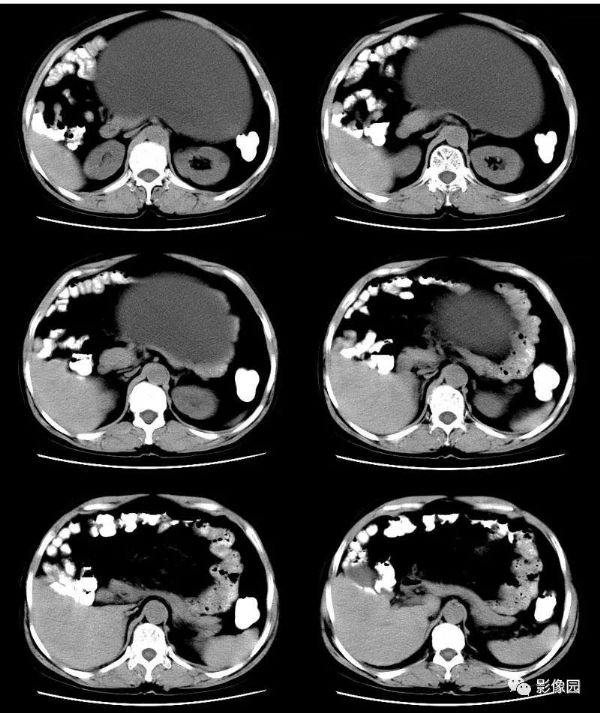
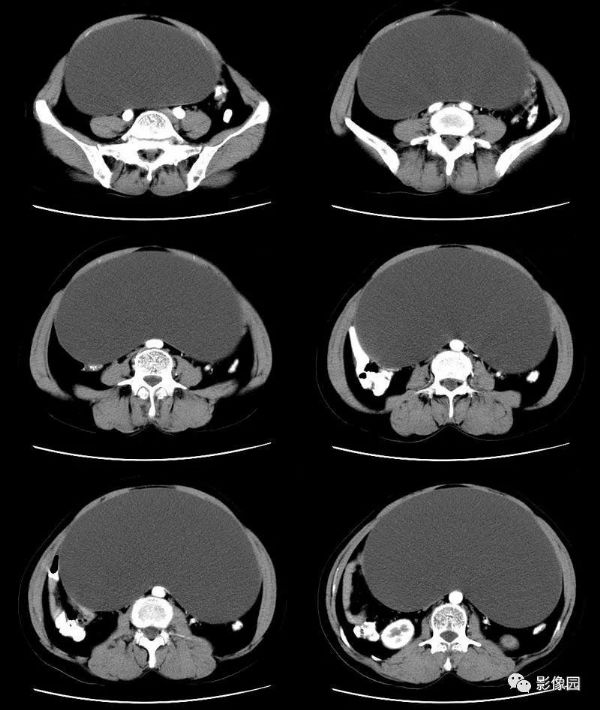
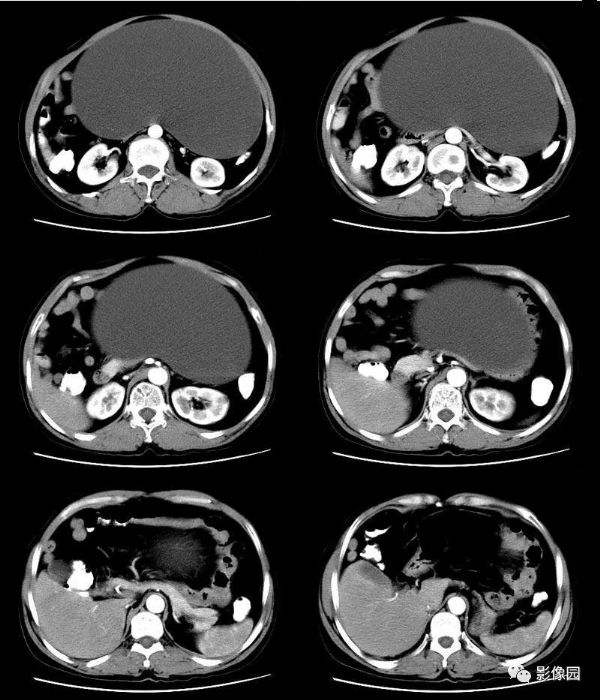
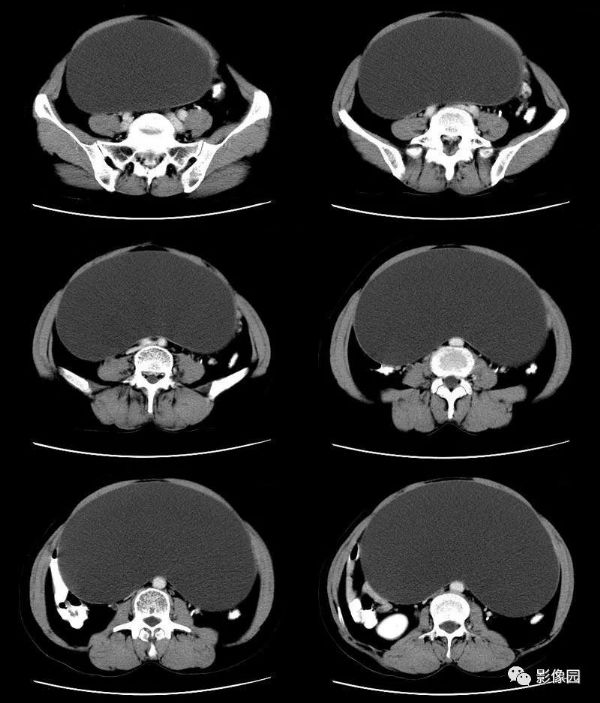
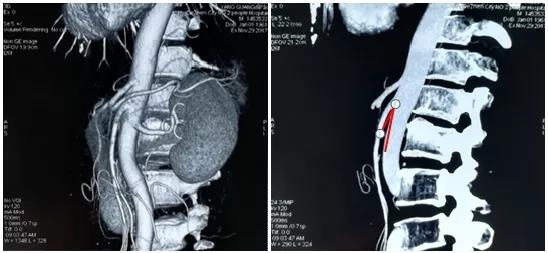
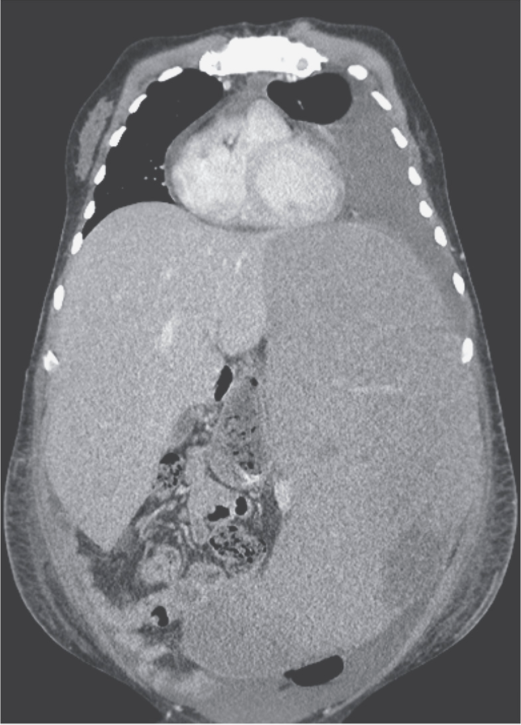
【影像图片】
【讨论】
评论:盆腔内巨大囊性占位病变,均匀薄壁,囊内无分隔,增强扫描无强化,考虑浆液性囊腺瘤可能大。
【病理结果】
符合卵巢粘液性囊肿
【病例小结】
卵巢粘液性囊腺瘤属于上皮性肿瘤,根据其细胞分化程度,区分为良性、交界性、恶性。多见于30~50岁妇女,大多为单侧性。肿瘤体积常较大,绝大多数为薄壁多房囊性,子囊多且大小不等,囊壁和间隔厚薄不均,少数呈单囊改变,囊壁稍厚,囊内密度不均,部分子囊密度较高,CT值在40-70HU间,酷似实性,这与粘液性囊腺瘤囊内含有较高蛋白成分或出血有关;部分子囊内可见孙囊,为特征性表现。增强扫描囊壁及间隔强化。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#并发#
78
#盆腔包块#
66
#腹盆腔#
62
#包块#
87
#腹胀#
61