Stroke:缺血性脑卒中患者缺血性病变体积与功能预后之间的关系!
2017-03-31 xing.T MedSci原创
由此可见,在脑卒中发病后24小时内ILV增长是很常见的。然而,24小时ILV证明是有价值的次要结局指标,它与发病后1周的ILV与功能预后之间的相关性一样强烈。
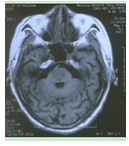
发病1周时的非对比CT上的缺血性病变体积(ILV)可以作为急性缺血性脑卒中患者次要的结局指标。发病24小时非对比CT上的ILV对功能结局的早期估计具有更高的可用性和潜在价值。近日,卒中领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在评估卒中发病后24小时病灶变化情况,以及比较了卒中后24小时和1周ILV与功能结局之间的相关性。
研究人员共纳入228例来自于荷兰急性缺血性卒中血管内治疗的多中心随机试验(MR CLEAN试验)的参与者,这些参与者接受在发病后24小时和1周进行了CT平扫,并进行了ILV测量。同时也对相对和绝对病变生长情况进行了测定。Logistic回归模型的构建纳入了24小时ILV或1周ILV。顺序和二分(0-2和3-6)的改良Rankin量表评分分别作为主要和次要结局指标。
发病后24小时和1周的中位ILV分别为42 ml(四分位间距范围为21-95ml)和64ml(四分位间距范围为30-120ml)。121例(53%)患者的相对病变增长超过30%,有83例(36%)患者绝对病变增长超过20ml。发病后24小时和1周ILVs两者具与功能预后显著相关(P均<0.001)。在logistic回归分析中,接受者操作特性曲线的曲线下面积24小时ILV和1周ILV是相似的分别为:0.85(95%可信区间为0.80-0.90)和0.87(95%可信区间为0.82-0.91)。
由此可见,在脑卒中发病后24小时内ILV增长是很常见的。然而,24小时ILV证明是有价值的次要结局指标,它与发病后1周的ILV与功能预后之间的相关性一样强烈。
原始出处:
Amber Bucker,et al. Associations of Ischemic Lesion Volume With Functional Outcome in Patients With Acute Ischemic Stroke.Stroke. 2017. https://doi.org/10.1161/STROKEAHA.116.015156
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#缺血性脑#
55
#脑卒中患者#
53
#缺血性#
52
#卒中患者#
46
#功能预后#
68
文章不错,值得分享
135
好。。。。。。
83
好。。。。。。
85