PLoS Med:荟萃分析二甲双胍治疗糖尿病的风险和效益
2012-04-12 Beyond 生物谷
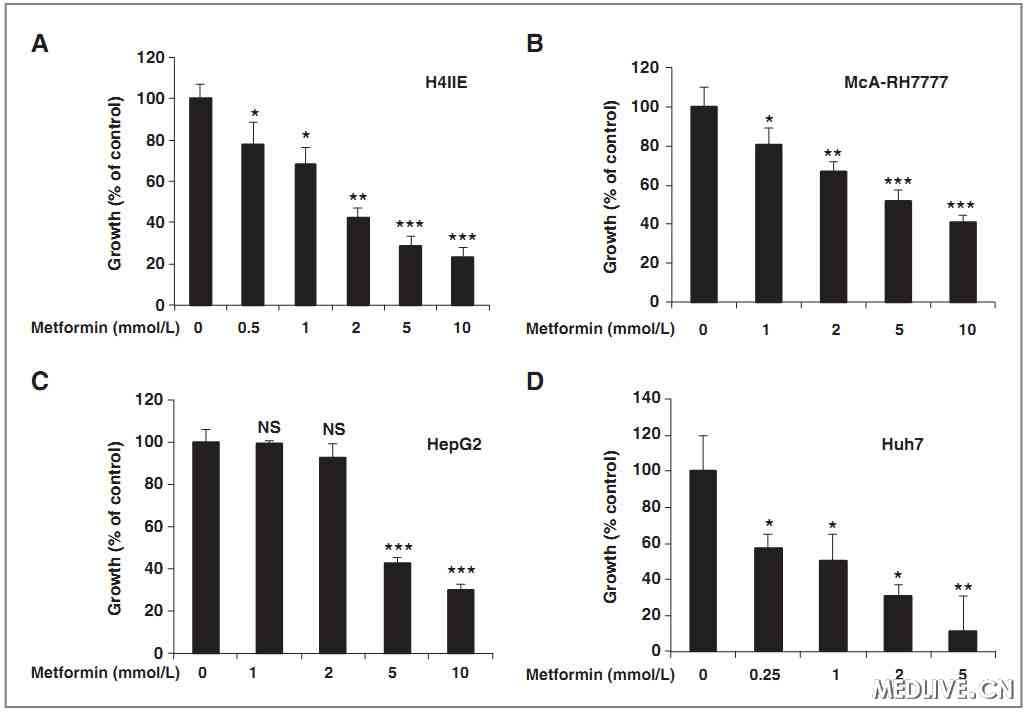
尽管该药物二甲双胍被认为是治疗2型糖尿病的代表药物,但近日法国研究人员开展的一项研究证实与存在的风险相比,这种药物的长期效益并没有被明确。目前,世界各地成千上万的人频繁服用二甲双胍以帮助控制自身血液中血糖水平,甚至有人认为服用二甲双胍对健康有长期的好处。相关研究论文发表在PLoS Medicine杂志上。 在过去14年中,二甲双胍被成为2型糖尿病一线治疗药物。当二甲双胍与饮食控制措施相结合时,二
尽管该药物二甲双胍被认为是治疗2型糖尿病的代表药物,但近日法国研究人员开展的一项研究证实与存在的风险相比,这种药物的长期效益并没有被明确。目前,世界各地成千上万的人频繁服用二甲双胍以帮助控制自身血液中血糖水平,甚至有人认为服用二甲双胍对健康有长期的好处。相关研究论文发表在PLoS Medicine杂志上。
在过去14年中,二甲双胍被成为2型糖尿病一线治疗药物。当二甲双胍与饮食控制措施相结合时,二甲双胍能降低超重2型糖尿病患者的死亡率。然而该研究发现二甲双胍对非超重的2型糖尿病患者而言,实际上可能会增加死亡的风险。
在这项新的荟萃分析研究中,法国里昂临床研究中心Catherine Cornu对所有相关研究提供的数据进行重新评估,评估服用二甲双胍2型糖尿病的风险与利益。
研究人员通过对13个随机对照试验(总共包括13,000多例患者)分析研究发现,与其他药物相比,二甲双胍对患者因各种原因死亡的风险或因心血管疾病死亡的风险并没有影响。此外,二甲双胍对患者发展患有心血管疾病如心脏病发作、中风以及心脏衰竭的风险没有显著影响。
作者总结说:“我们有理由怀疑使用二甲双胍可能会增加或减少患者因各种原因死亡的风险或因心血管疾病死亡的风险”。
他们解释说:“目前研究尚未能证明二甲双胍防止死亡或心血管事件有具体疗效,因为现有研究的数量和质量是不够的”。

doi:10.1371/journal.pmed.1001204
PMC:
PMID:
Reappraisal of Metformin Efficacy in the Treatment of Type 2 Diabetes: A Meta-Analysis of Randomised Controlled Trials
Rémy Boussageon1, Irène Supper1, Theodora Bejan-Angoulvant2,3, Nadir Kellou1, Michel Cucherat4,5, Jean-Pierre Boissel4,5, Behrouz Kassai4,5,6,7, Alain Moreau1, Fran?ois Gueyffier4,5,6,7, Catherine Cornu4,5,6,7*
This meta-analysis of randomised controlled trials evaluated metformin efficacy (in studies of metformin versus diet alone, versus placebo, and versus no treatment; metformin as an add-on therapy; and metformin withdrawal) against cardiovascular morbidity or mortality in patients with type 2 diabetes. We searched Medline, Embase, and the Cochrane database. Primary end points were all-cause mortality and cardiovascular death. Secondary end points included all myocardial infarctions, all strokes, congestive heart failure, peripheral vascular disease, leg amputations, and microvascular complications. Thirteen randomised controlled trials (13,110 patients) were retrieved; 9,560 patients were given metformin, and 3,550 patients were given conventional treatment or placebo. Metformin did not significantly affect the primary outcomes all-cause mortality, risk ratio (RR) = 0.99 (95% CI: 0.75 to 1.31), and cardiovascular mortality, RR = 1.05 (95% CI: 0.67 to 1.64). The secondary outcomes were also unaffected by metformin treatment: all myocardial infarctions, RR = 0.90 (95% CI: 0.74 to 1.09); all strokes, RR = 0.76 (95% CI: 0.51 to 1.14); heart failure, RR = 1.03 (95% CI: 0.67 to 1.59); peripheral vascular disease, RR = 0.90 (95% CI: 0.46 to 1.78); leg amputations, RR = 1.04 (95% CI: 0.44 to 2.44); and microvascular complications, RR = 0.83 (95% CI: 0.59 to 1.17). For all-cause mortality and cardiovascular mortality, there was significant heterogeneity when including the UK Prospective Diabetes Study subgroups (I2 = 41% and 59%). There was significant interaction with sulphonylurea as a concomitant treatment for myocardial infarction (p = 0.10 and 0.02, respectively).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#荟萃分析#
65
#荟萃#
54
#Med#
62