BMJ:轻微跌倒后肩部疼痛恶化后发现了肺癌-案例报道
2017-02-16 xing.T MedSci原创
病人进行胸部和腹部CT扫描以及随后进行的肺活检,发现为T2N0M0原发性肺腺癌。该患者接受手术切除,病人在两年内安然无恙。
患者为一名62岁男性,因在轻微跌倒后肩部疼痛恶化而就诊。医生要求进行X线检查,根据患者X线检查结果(如图1所示),下一步该怎么做?
图1右肩前后位平片
答案
进行胸部和上腹部计算机断层扫描(CT)检查。肩关节X线片显示空泡肺结节,测量其大小约2厘米(如图2所示)。这最有可能是原发性肺癌,并应转诊到肺癌多学科团队就诊。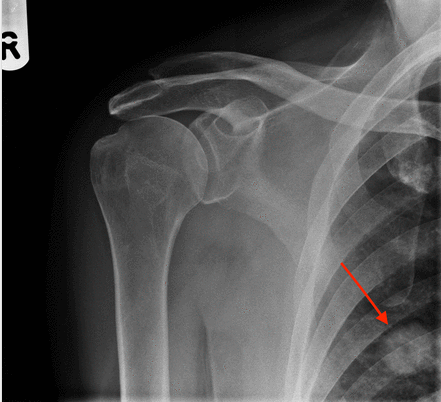
图2右肩前后位平片,右肺有空泡肺结节(红色箭头
学习要点
当看到一个孤立的肺结节,请肺癌多学科团队进行适当的进一步调查。
患者预后
病人进行胸部和腹部CT扫描以及随后进行的肺活检,发现为T2N0M0原发性肺腺癌。该患者接受手术切除,病人在两年内安然无恙。
原始出处:
Lauren Ramsay,et al. Sharp shoulder pain, getting worse, after a fall.BMJ 2017; 356 doi: https://doi.org/10.1136/bmj.j571
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
56
这个病例有啥稀罕的,一抓一大把
96
好文,值得点赞,值得拥有,值得收藏!
99