JCI:治疗深静脉血栓的新方法
2014-07-07 佚名 不详
项研究发现去除酶因子ⅩⅢ,能降低血凝块中红细胞的数量,导致凝块的大小减少了50%。这一发现发表在Journal of Clinical Investigatio杂志上,对深静脉血栓(DVT)高风险的人有重大影响。 论文作者Alisa Wolberg博士表示:如果我们能够利用这一发现,以减少血液凝块的大小,这将意味着一个全新的方法来治疗血栓。我们认为降低ⅩⅢ因子活性可帮助一大批人,包括那些无法
项研究发现去除酶因子ⅩⅢ,能降低血凝块中红细胞的数量,导致凝块的大小减少了50%。这一发现发表在Journal of Clinical Investigatio杂志上,对深静脉血栓(DVT)高风险的人有重大影响。
论文作者Alisa Wolberg博士表示:如果我们能够利用这一发现,以减少血液凝块的大小,这将意味着一个全新的方法来治疗血栓。我们认为降低ⅩⅢ因子活性可帮助一大批人,包括那些无法利用现有的“血液稀释”药物的人。血液凝结能力对我们的健康至关重要,通过阻止出血,使伤口愈合,血栓让我们避免受伤流血而死。但在错误的情况下,凝块可能会造成显著健康危害。
深静脉血栓患者,血管内形成血栓,通常导致两腿瘫痪,阻碍血液的流动,从而导致疼痛、肿胀。许多患者经常服用血液稀释药物如华法林,但这扼杀了身体生成纤维蛋白的能力。这些药物提高出血过多的危险,可引起副作用,并且不适合于所有的患者。
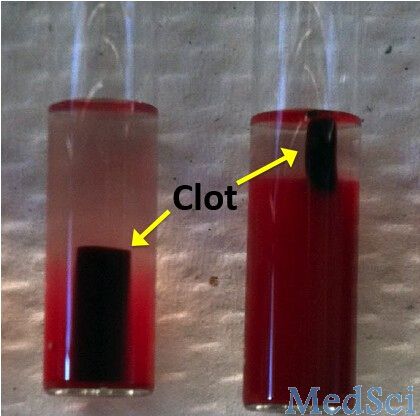
我们需要的是一种药物降低了形成大的血凝块的风险,但仍然可以让你拥有形成血块的能力(当出血的时候),Wolberg说:我们已经发现可能使人们有可能取得这种平衡的生物途径。在利用老鼠和人类的血液实验中,研究人员研究了ⅩⅢ因子蛋白在血块形成中的作用。令他们吃惊的是,他们发现,不能产生ⅩⅢ因子的小鼠虽然也能形成血凝块,但大小是正常小鼠形成血凝块的一半大小。
然后,研究发现,大小差异实际上是由于血块中红细胞的数量减少导致的。因子XIII似乎在形成凝块中,帮助纤维蛋白基质保持其完整性起到了至关重要的作用。正常情况下,血纤蛋白基质在凝块内部和周围形成了一个强有力的网格,捕获红细胞。无因子XIII后,一些红血细胞被挤压出来,导致一个更小的血块。不同于现有的以减少纤维蛋白药物,也许将来一种降低凝血因子XIII药物可能会削减人体产生大量的,危险的血块能力,但不牺牲生成小的,有利于血栓形成的血块的能力。
原始出处
Aleman MM, Byrnes JR, Wang JG, Tran R, Lam WA, Di Paola J, Mackman N, Degen JL, Flick MJ, Wolberg AS.Factor XIII activity mediates red blood cell retention in venous thrombi.J Clin Invest. 2014 Jul 1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









静脉血栓
54
看看下
134
#新方法#
55
#静脉#
54
#静脉血#
0
#JCI#
52