Int J Cardiol:非阻塞性冠状动脉心肌梗死人群水平的发生率和结局分析!
2018-04-06 xing.T MedSci原创
由此可见,MINOCA人群水平的发病率约为5%。尽管他们的解剖发现是良性的,但必须努力改善二级预防策略,以减轻这一人群长期不良后果的负担。
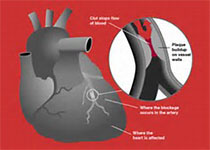
非阻塞性冠状动脉心肌梗死(MINOCA)是一种已知的临床难题,对其的调查也十分有限。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,通过一个大型的以人群为基础的队列,研究人员评估了MINOCA的发生率、人口状况、循证医学情况和患者临床结局。
研究人员招募了在加拿大阿尔伯塔202年4月1日至2014年3月31日期间接受冠状动脉造影的初步诊断为MI的患者。并对MINOCA患者与阻塞性冠状动脉疾病(OCD)患者之间进行了比较。该研究的主要复合终点为1年全因死亡或再MI。
在35928例MI患者中,2092例(5.8%)为MINOCA患者。其中MINOCA患者的住院死亡率为0.8%,OCD患者的住院死亡率为2.7%(P<0.0001)。在6月时,MINOCA患者的心血管循证医学使用率显著低于OCD患者。一年死亡/再MI率在MINOCA患者为5.3%,而OCD患者为8.9%(调整后的风险比(aHR)为0.75,95%可信区间(CI)为0.62–0.92,P<0.0001)。MINOCA患者与OCD患者的五年病死率分别为10.9%和16%。经进一步分层,770例(36.8%)MINOCA患者没有CAD的血管造影证据(即正常血管造影)。这些患者的循证医学使用率甚至更低。一年死亡/再MI率在这些患者中为3.9%,相比于狭窄<50%的MINOCA患者为6.1%(Ahr为0.68,95%CI为0.44–1.07,P=0.028)。
由此可见,MINOCA人群水平的发病率约为5%。尽管他们的解剖发现是良性的,但必须努力改善二级预防策略,以减轻这一人群长期不良后果的负担。
原始出处:
Kevin R. Bainey,et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA): Insights from the Alberta contemporary acute coronary syndrome patients invasive treatment strategies (COAPT) study.International Journal of Cardiology.2018. https://doi.org/10.1016/j.ijcard.2018.04.004
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cardiol#
74
#发生率#
74
#阻塞#
59
学习了.谢谢作者分享!
104
好
74
好文章.学习获益匪浅.
89
学习了.长知识
74