Eur Radiol:钆塞酸二钠增强MRI的肝癌术后预后评估是否可应用于多中心?
2021-03-13 shaosai MedSci原创
肝细胞肝癌(HCC)一直是重要的全球性健康问题,在世界范围内发病率正在不断上升。对于具有良好肝功能的孤立性HCC患者,手术切除和消融都是主要的治疗方法.

肝细胞肝癌(HCC)一直是重要的全球性健康问题,在世界范围内发病率正在不断上升。对于具有良好肝功能的孤立性HCC患者,手术切除和消融都是主要的治疗方法,而手术切除还可以提供例如肿瘤大小、分化程度和血管浸润情况等肿瘤分期的预后信息。即使对于多发性HCC患者来说,手术切除也比非手术治疗提供了更好的生存机会。在当前的美国癌症联合委员会(AJCC)分期系统的第8版中,根据最大肿瘤的大小,多发性HCC患者被归为T2期或T3期。除肿瘤大小外,多发性HCC患者还需要进一步评价其他预后因素。
多期CT和MRI检查已被多项研究证明在肝癌的检测、表征和分期中起着重要作用。多发HCC可以通过两种不同的机制,其一为多中心HCC的独立致癌作用,或者为原发性HCC的肝内转移。当肝内转移结节小于2 cm,距较大的主要肿瘤小于2 cm,并且与主要肿瘤的距离大于结节直径时,则认为该结节为卫星灶。尽管当前的第8版AJCC分期系统并未对卫星灶、HCC肝内转移及多中心性HCC进行区分,但已有研究证明HCC肝内转移患者的预后明显差于多中心性HCC患者,因此对多发HCC进行鉴别对于临床护理至关重要。
近日,发表在European Radiology杂志的一项研究明确了多中心多发性肝细胞癌(HCC)手术切除术后的患者的临床和组织病理学预后因素,并评价了特定的影像学相关因素(包括动脉期明显强化(APHE)和钆塞酸二钠增强MRI上每个病变的LI-RADS类别)在诊断多中心HCC时可提供的额外的预后信息。
本项回顾性研究共纳入2009年至2014年间在一家三级医院通过手术切除术诊断为肝癌的54位患者共120个多中心性肝癌病灶。两名独立阅读者评价了患者术前钆塞酸二钠增强MR的图像并记录了每个HCC病灶的APHE和LI-RADS类别 。如有必要,可通过共识会议解决差异。 使用Cox回归分析分析了预测无病生存期(DFS)和总体生存期(OS)的潜在临床病理和影像学参数。
微血管浸润(MVI)(p = 0.003)和三个或更多HCC(p = 0.013)病灶的存在都是较短DFS的独立预测因素。 并发MVI和三个或更多HCC的患者DFS最短。MVI是预测OS的唯一具有统计学意义的参数(p = 0.023)。 APHE或LR-5 / M类肝癌的数量与生存率无关。

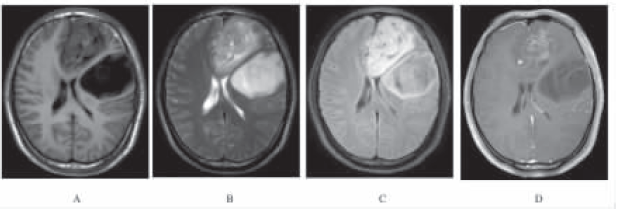
图1 基于微血管浸润(MVI)和多中心性HCC数量的Kaplan-Meier生存曲线。有MVI患者的(a)无病生存期(DFS)和(b)总生存期(OS)明显短于无MVI患者。(c)有3个或更多HCC患者的DFS明显短于有2个HCC的患者。(d)有MVI与3个或3个以上HCC的生存曲线相互重叠。MVI组和3个及以上HCC组均较MVI组和3个及以上hcc组DFS短,p值分别为0.046和0.068。

图2 基于LI-RADS分类和APHE的两个病灶的多中心性HCC患者的Kaplan-Meier生存曲线。(a)无病生存期和(b)总生存期(OS)不受两个HCC是否均为LR-5/M分类或至少一个HCC为LR-3/4的显著影响。DFS (c)和OS (d)不受两个HCC或至少一个HCC不存在APHE的显著影响。
MVI和3个或3个以上的肝癌是多中心性HCC癌手术切除后DFS较短的独立预测因子。MVI是OS较差的唯一显著预测因子。每个HCC的钆塞酸二钠增强MRI影像学表现(如APHE或LI-RADS分类)均与多中心性HCC患者的术后复发或生存率无关。
原始出处:
Seung-Seob Kim,Sunyoung Lee,Myeong-Jin Kim.et al. Prognostic factors of gadoxetic acid-enhanced MRI for postsurgical outcomes in multicentric hepatocellular carcinoma.PMID:33146795DOI:10.1007/s00330-020-07419-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#预后评估#
84
#钆塞酸二钠#
62
#多中心#
70
好
111
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
72
真好!
100