JAHA:基底动脉直径的变化与心血管事件发生呈负相关
2019-02-25 不详 MedSci原创
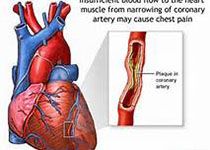
基底动脉(BA)的扩张被认为是心血管事件(CVEs)发生的预测因子,然而 ,BA直径的纵向变化(ΔBA)是否与CVEs相关尚不清楚。首先,本研究对493例患者采用时间依赖性Cox比例风险模型进行分析,以评估ΔBA和CVES之间的相关性。其次,通过线性回归分析,本研究评估了164名接受长期随访磁共振成像的患者的纵向ΔBA。经过平均8.7年时间的随访,有105例患者发展为CVEs,较小的Δba与高CV
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血管事件#
63
#AHA#
68
#基底动脉#
63
#负相关#
62