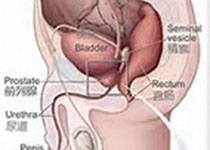
Oncogene: CRIPTO和它的信号伴侣GRP78能促使人类前列腺癌骨转移表型
2017-04-16 AlexYang MedSci原创
CRIPTO (CR-1,TDGF1)是一个细胞表面/分泌的肿瘤蛋白并积极的参与发育和癌症。最近,研究人员报道了CRIPTO的高表达与前列腺癌(PCa)患者分层风险组的低生存率有关。研究结果发现,CRIPTO和它的信号伴侣-葡萄糖调节的蛋白78(GRP78)在PCa转移肿瘤中高度表达,并且与非转移性ALDHlow比较,在PC-3M-Pro4Luc2 PCa 细胞的转移性ALDHhigh亚群中有着更
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Gene#
56
感谢分享一下!
102
#表型#
44
#Oncogene#
62
#伴侣#
57