Liver Cancer:不可切除肝细胞癌患者基线肝功能和预后的关系:来自3期临床研究REFLECT患者的分析结果
2021-07-16 yd2015 MedSci原创
不可切除肝细胞癌患者使用仑伐替尼或索拉非尼治疗时,基线较好的肝功能(比如ALBI分级或CPS评分)可能是预测较好生存的预后指标。
REFLECT研究是一项全球、随机、开放标签、III期临床研究,评估仑伐替尼(Lenvatinib)对比索拉非尼(sorafenib)一线治疗不可切除肝细胞癌(uHCC)患者的疗效。研究表明仑伐替尼非劣效于索拉非尼。中位OS为13.6 个月 (95% CI, 12.1–14.9)对比12.3个月(95%CI,10.4–13.9) [HR=0.92; 95%CI, 0.79–1.06]。另外仑伐替尼较索拉非尼明显延长PFS,为7.4 个月(95%CI,6.9–8.8) 对比3.7个月 (95% CI, 3.6–4.6)],以及ORR为24.1% (95% CI, 20.2–27.9)对比9.2% (95% CI, 6.6–11.8)。研究者对REFLECT研究的患者进行探索,评估不可手术切除肝细胞癌(HCC)患者的基线肝功能Child-Pugh评分(CPS)以及白蛋白-胆红素分级(ALBI)与仑伐替尼或索拉非尼治疗的疗效和安全性的关系。相关研究结果发表在Liver Cancer杂志上。
该研究只纳入ALBI 1级或2级和CPS 5级或6级接受lenvatinib或sorafenib的患者。CPS评分采用血清胆红素、血清白蛋白、腹水、脑病、INR等5项指标计算。根据严重程度的增加给每个标准打分,总值最低(即5)表示肝损害最小。只有白蛋白和胆红素被用于计算晚期ALBI评分,使用线性预测公式= (log 10 bilirubin x 0.66) +(白蛋白x0.085),其中胆红素以mol/L为单位,白蛋白以g/L为单位。评分分为1 - 3级:≤-2.60(1级),>-2.60和≤-1.39(2级), >-1.39(3级),1级表示肝损害最小。
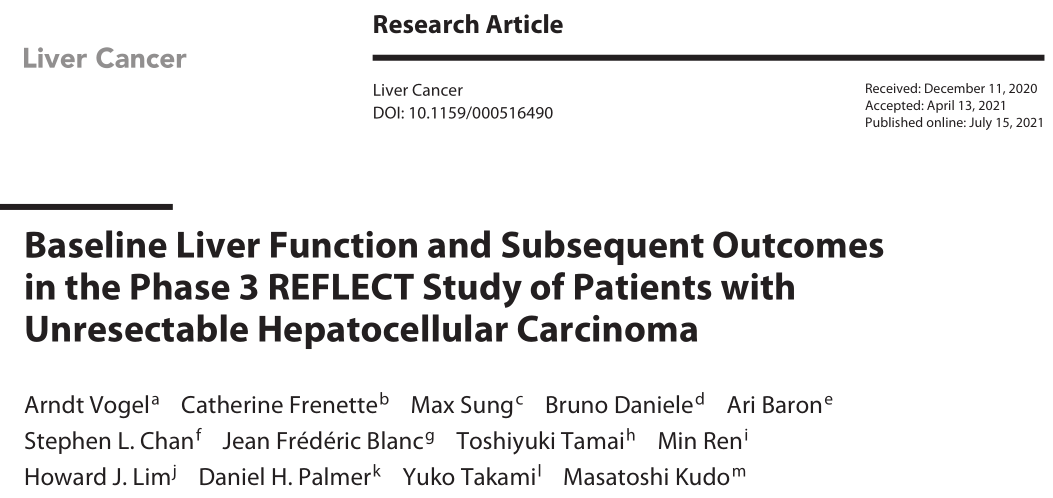
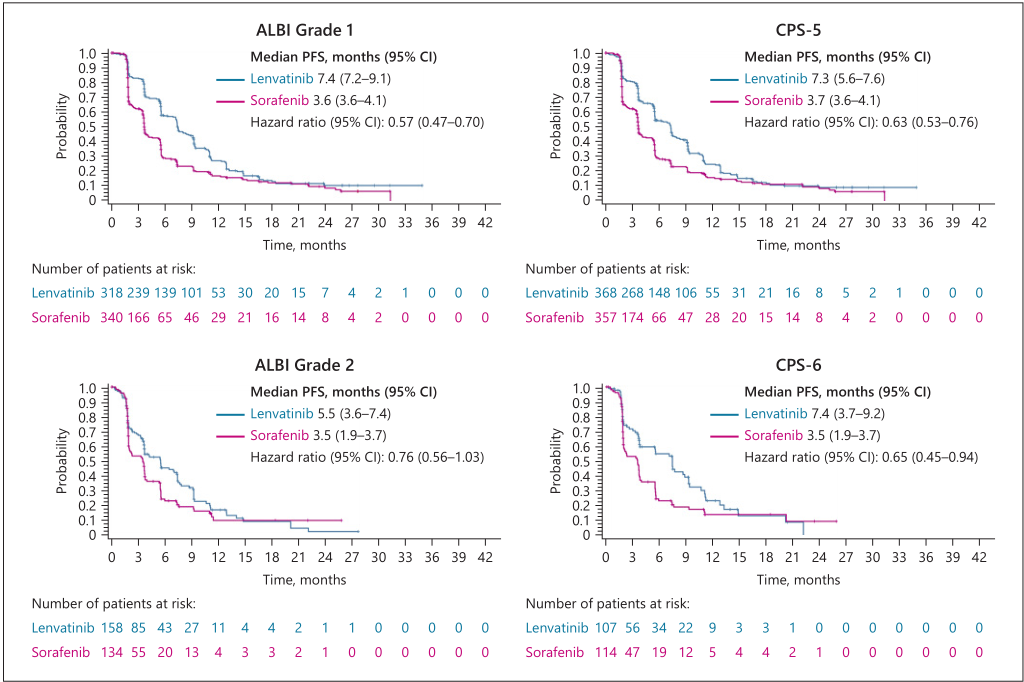
ALBI 1级患者,接受仑伐替尼和索拉非尼的中位OS分别为17.4个月 (95% CI: 14.1–19.8)和14.6个月(95% CI: 12.5–16.9);ALBI 2级患者,接受仑伐替尼和索拉非尼的中位OS分别为8.6个月 (95% CI: 7.0–11.5)和7.7个月(95% CI: 6.1–10.2)。CPS 5分患者,接受仑伐替尼和索拉非尼的中位OS分别为15.3个月(95%CI: 13.4–18.2)和14.2 个月(95% CI: 12.0–16.3);CPS 6分患者,接受仑伐替尼和索拉非尼的中位OS分别为9.4个月(95% CI: 7.0–12.1) 和 7.9个月(95% CI: 6.3–11.7)。
OS
仑伐替尼治疗后接受后续抗肿瘤治疗的患者中,ALBI 1级(n = 158)患者的中位OS为20.9个月(95% CI: 17.6–25.9), ALBI 2级 (n = 46)患者中位 OS 为15.1个月(95% CI: 12.2–20.8; HR 0.643, 95% CI: 0.440–0.938)。
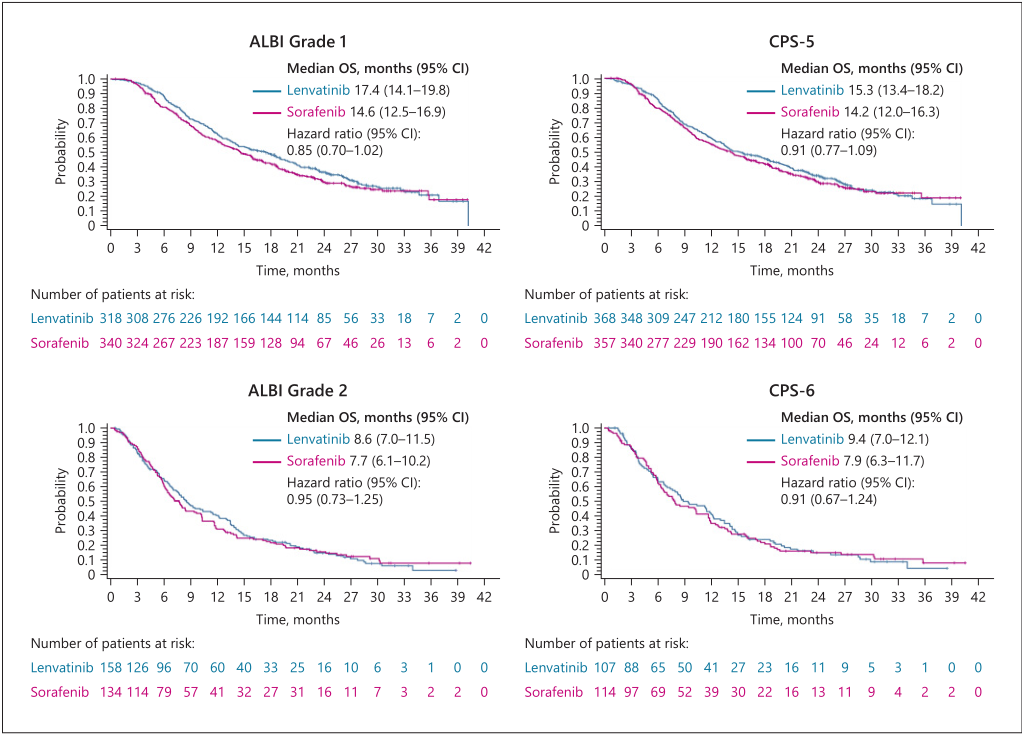
ALBI 1级患者,接受仑伐替尼和索拉非尼的中位PFS分别为7.4个月 (95% CI: 7.2–9.1)和3.6 个月(95% CI: 3.6–4.1);ALBI 2级患者,接受仑伐替尼和索拉非尼的中位PFS分别为5.5个月(95% CI: 3.6–7.4)和3.5个月(95%CI: 1.9–3.7)。CPS 5分患者,接受仑伐替尼和索拉非尼的中位PFS分别为7.3个月(95% CI: 5.6–7.6)和3.7 个月(95% CI: 3.6–4.1);CPS 6分患者,接受仑伐替尼和索拉非尼的中位PFS分别为7.4个月(95% CI: 3.7–9.2) 和 3.5个月(95% CI: 1.9–3.7)。
PFS
仑伐替尼治疗的患者,ALBI 1级和2级患者的ORR分别为 45.0%和32.3%;CPS 5分和6分的ORR分别为42.9% 和 33.6%。索拉非尼治疗的患者,ALBI 1级和2级患者的ORR分别为 13.8%和9.0%;CPS 5分和6分的ORR分别为14.0% 和7.9%。
疗效评估
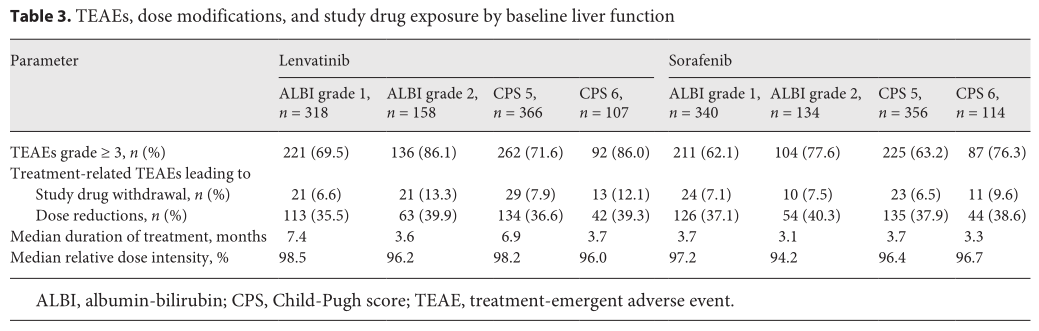
仑伐替尼治疗的患者,ALBI 1级和2级患者出现≥3 级治疗相关不良事件(TEAE)的比例分别为 69.5%和 86.1%;而CPS 5分和6分患者的分别为71.6%和 86.0%。索拉非尼治疗的患者,ALBI 1级和2级患者出现≥3 级治疗相关不良事件(TEAE)的比例分别为 62.1%和77.6%;而CPS 5分和6分患者的分别为63.2%和 76.3%。
治疗不良事件
综上,不可切除肝细胞癌患者使用仑伐替尼或索拉非尼治疗时,基线较好的肝功能(比如ALBI分级或CPS评分)可能是预测较好生存的预后指标。
原始出处:
Arndt Vogel, Catherine Frenette , Max Sung, et al. Baseline Liver Function and Subsequent Outcomes in the Phase 3 REFLECT Study of Patients with Unresectable Hepatocellular Carcinoma. Liver Cancer. DOI: 10.1159/000516490. Published online: July 15, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞癌#
46
#肝细胞#
54
#3期临床#
74
#肝功能#
72
学习了
72