常见不典型病例赏析--髋关节色素绒毛结节性滑膜炎(摘自华夏周一读片)
2022-09-17 华夏影像诊断中心 华夏影像诊断中心
MRI检查表现:在T1和T2加权像上,含铁血黄素都表现为低信号或无信号。PVNS最典型的MRI特点是在T1、T2以及质子像上均表现为关节内低信号的结节性肿块。
简要病史:男,27岁,因“发现左髋部内侧包块3天”入院。
病例特点:
1.男性27岁患者,无明显外伤史。
2.入院情况:患者自诉3天前运动后出现左髋部疼痛,无局部红肿,无下肢麻木,无明显活动障碍,于当地卫生室就诊后怀疑为“疝气”,2014-04-24转入我院门诊就诊,门诊即以左髋部性变收住院。患者起病以来精神尚可,体力正常,食欲正常,睡眠正常,体重无明显变化,大便正常,排尿正常。
3.平素健康状况良好,曾由于右腓骨骨折行手术治疗,已愈合。否认外伤史,否认输血史,自诉有青霉素过敏史,表现为皮疹、食物过敏史,预防接种随当地进行。
影像资料: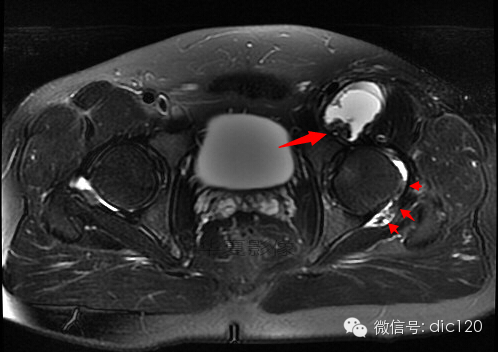
T2WI序列左侧髋关节滑膜囊内及髂腰肌滑囊内低信号含铁血黄素信号。
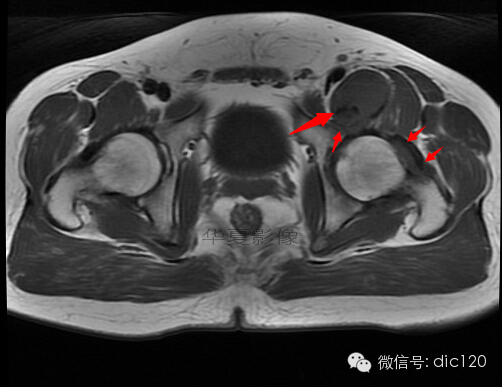
T1WI序列髂腰肌滑囊内低信号含铁血黄素信号,左侧髋关节囊少量液体
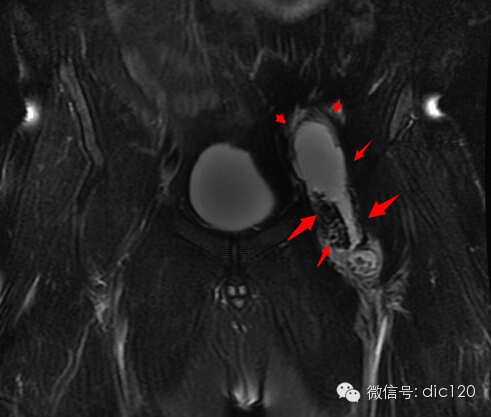
冠状位T2FS序列髂腰肌滑囊囊肿

T1压脂增强序列左侧髋关节滑膜明显增厚强化,其内细小绒毛状结构
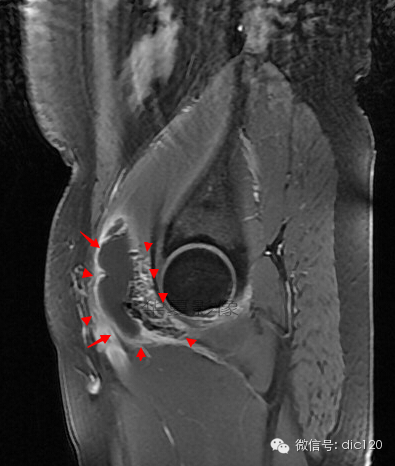
矢状位T1压脂增强序列,示囊肿及含铁血黄素成分、绒毛状结构

冠状位T1压脂增强序列,图示囊肿及含铁血黄素成分、绒毛状结构
手术病理:
大体标本:已破囊肿一个6x4.5x2cm,壁厚0.1-0.5cm,质软,囊内壁灰黄色,另见灰黄、淡黄碎组织一堆5x4.5x0.5cm,切面灰黄,质软。
印象:(左髋关节)色素绒毛结节性滑膜炎并滑膜囊肿。
讨论:色素沉着绒毛结节性滑膜炎(PVNS)是滑膜的一种增生性病变,经常表现为局限的结节。肿块可能起源于关节滑膜、腱鞘、筋膜层或韧带组织。病变表现为无痛性软组织肿块,通常位于手指和足趾处。也可见于其他关节。
病因:病因不明,说法不一。总结起来,主要有以下4种:①脂质代谢紊乱;②创伤及出血;③炎症;④肿瘤。
临床常表现:关节的无痛肿胀或轻度疼痛伴肿胀。偶尔可以出现急性的关节疼痛和肿胀。患者还可能出现关节绞锁等症状。对于年轻患者出现的难以解释的髋部疼痛应考虑有PVNS的可能。PVNS有两种表现形式:弥漫型和结节型。结节型最常见于手部,弥漫型最常见于膝关节。
MRI检查表现:在T1和T2加权像上,含铁血黄素都表现为低信号或无信号。PVNS最典型的MRI特点是在T1、T2以及质子像上均表现为关节内低信号的结节性肿块。病变滑膜和灶性肿块在T2加权像上显示最好,表现为低信号区。这是由于含铁血黄素沉积造成的。在T1加权像上病变呈低信号。出血性滑膜炎可能会与PVNS混淆。
鉴别诊断
1.弥漫性色素沉着绒毛结节性滑膜炎必须与特发性滑膜骨软骨瘤病(可见钙化与骨化)、感染以及其他关节病变相鉴别。
2.与类风湿关节炎(RA)相鉴别,RA往往侵犯多关节,PVNS通常表现为单关节的出血性关节炎。单关节发病是PVNS的一个规律,但也有罕见的多关节病变。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
116
感谢分享
71
#不典型#
93
#色素#
0
#结节性#
68
#滑膜炎#
82