
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-03-14 佚名 中国临床医学影像杂志
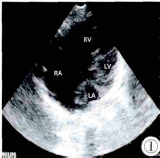
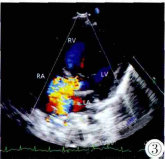
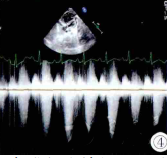
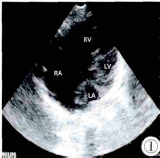
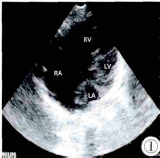
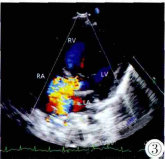
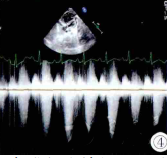
患儿,男,91d,外院示心脏超声异常入院


肺静脉分离(PVI)的基石是导管消融心房颤动(AF)。未行静脉间嵴消融(IVR)可能被纳入消融策略来实现肺静脉分离(PVI),然而,这种分离术的试验缺乏。研究人员进行了一项随机多中心研究旨在比较了最小(仅行环前庭PVI)与最大(环前庭PVI联合IVR消融)分离策略的疗效。研究人员收纳了234名阵发性房颤患者(平均59岁,66%男性),并比较了最小(仅行环前庭PVI)与最大(环前庭PVI联合IVR消
近期,阜外医院侯剑峰等对该院563例完全性肺静脉异位引流患者围手术期死亡危险因素进行了分析。
导管消融已成为心房颤动的有效治疗手段,,但心律失常复发很常见。腺苷测试可能识别房颤患者休眠肺静脉传导可减少心律失常复发。本研究明确静注腺苷能否识别肺静脉休眠传导并使阵发性房颤患者免于复发。 研究人员在澳大利亚和北美18所医院进行了这项随机对照试验。研究人员收纳了年龄大于18岁的534名6个月内房颤症状性发作≥3次的患者。患者于肺静脉分离后接受静注腺苷治疗以识别休眠传导。研究者随机选择如一些无休眠
澳大利亚一项研究表明,在阵发性房颤患者中,通过最小和最大消融策略实现肺静脉隔离(PVI)所得到的患者转归相同。但需要通过静脉间嵴(IVR)消融实现PVI的心房颤动(AF)患者复发率增加,造成此差异的一部分原因可能为解剖学上的差异。 此项研究共纳入200例年龄为59±9岁的阵发性房颤患者(患AF 60±55个月,左心房面积24.6±5.9cm2),并随机通过最小或最大消融策略实现环
由此可见,切除的非小细胞肺癌患者PPB和IPVB中CTC计数是TFS和OS的一个独立危险因素。


梅斯医学MedSci APP
医路相伴,成就大医
#重度主动脉瓣狭窄#
67
#静脉#
54
#主动脉瓣#
66
#主动脉#
55